Arkansas Blue Cross Blue Shield Prior Authorization Form
Arkansas Blue Cross Blue Shield Prior Authorization Form - Annual notice of changes (anocs) Arkansas blue cross and blue shield. Web make changes to existing membership. Web prior authorization is a process though which arkansas blue cross and blue shield approves a request for a covered healthcare service before the member receives the. Review the prior authorizations section of the provider manual. Send this form to your human resources office. Approval information for radiological services Prior authorization criteria is available. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website.
Annual notice of changes (anocs) Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. For more information about pharmacy prior approval and the required forms visit the prior approval page. Approval information for radiological services Web prior authorization is a process though which arkansas blue cross and blue shield approves a request for a covered healthcare service before the member receives the. Providers who are requesting a prior approval. Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Web select your county on the map below to see plan forms and documents. Prior authorization criteria is available. Web make changes to existing membership.
For more information about pharmacy prior approval and the required forms visit the prior approval page. Web medicare advantage prior authorization request form instructions: Approval information for radiological services Prior authorization criteria is available. Web make changes to existing membership. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Providers who are requesting a prior approval. Send this form to your human resources office. Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Web select your county on the map below to see plan forms and documents.
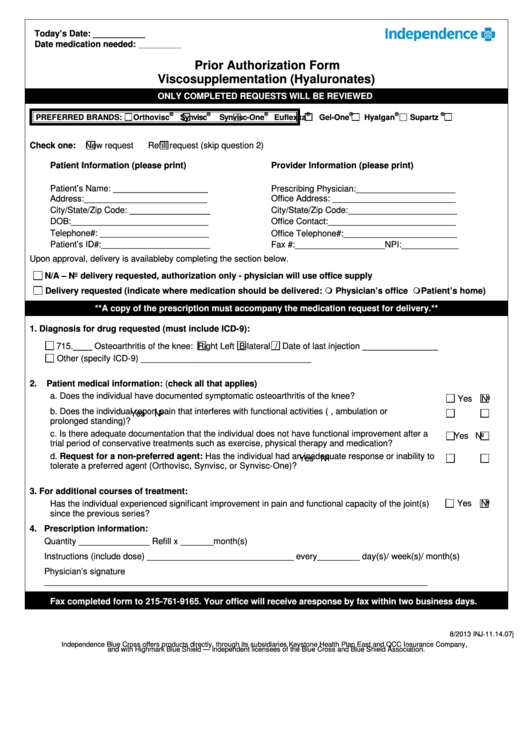
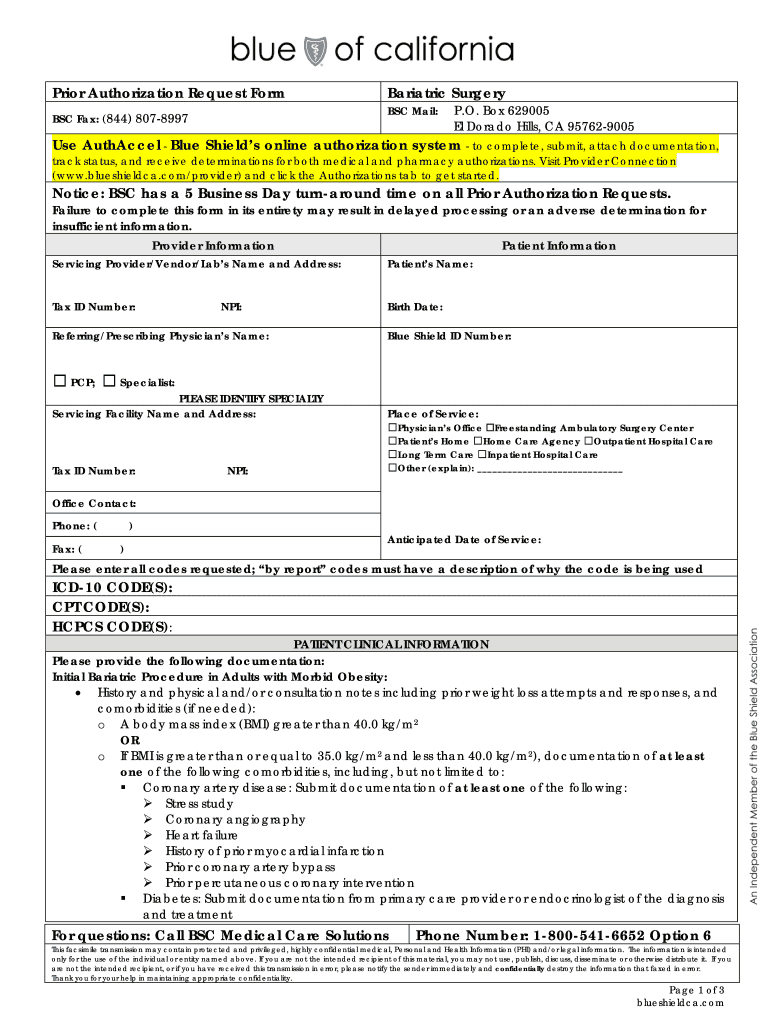
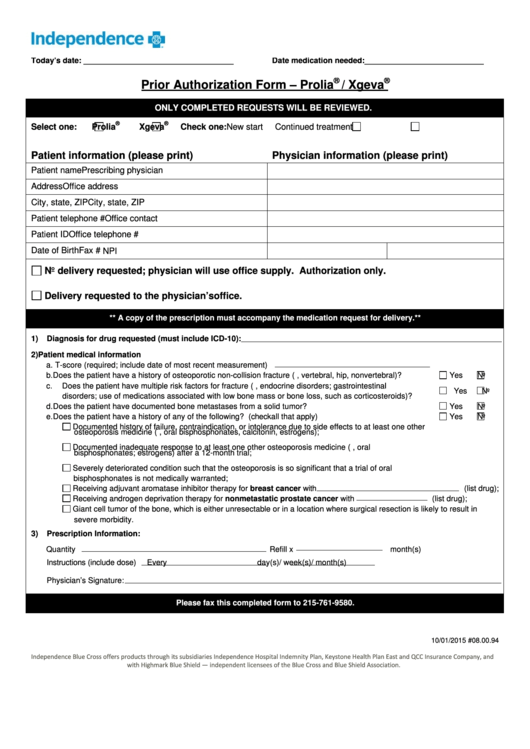
Independence Prior Authorization Form Viscosupplementation
Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Annual notice of changes (anocs) For more information about pharmacy prior approval and the required forms visit the prior approval page. Approval information for radiological services Web medicare advantage prior authorization request form instructions:
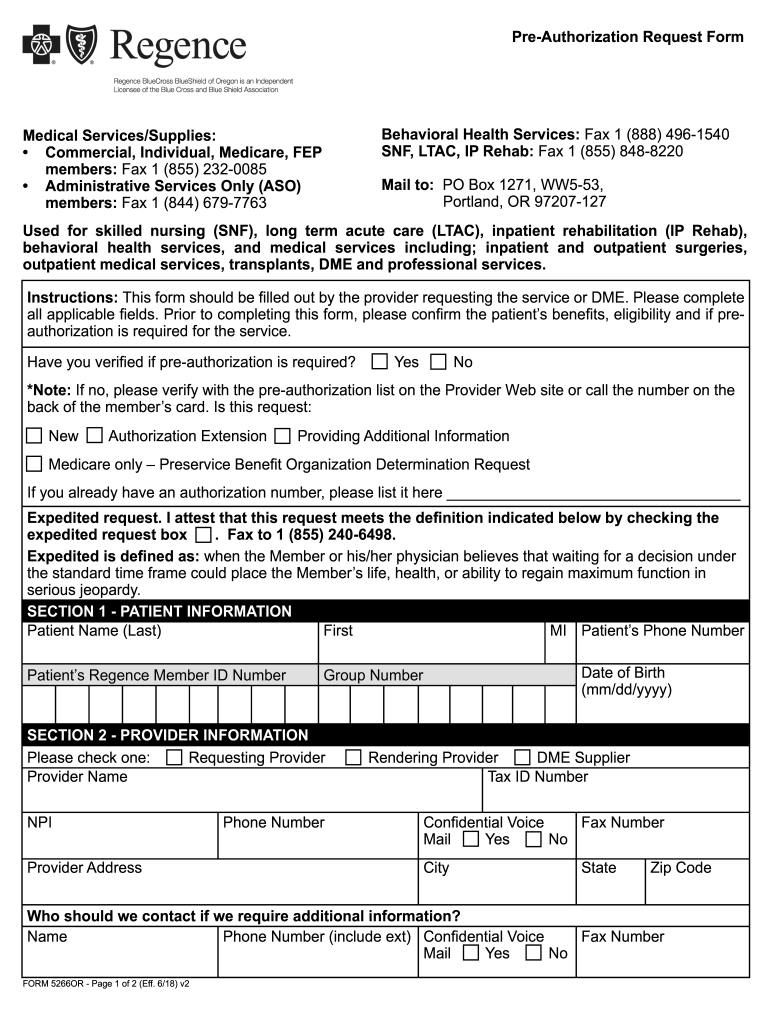
Bcbs Oregon Prior Authorization Fill Out and Sign Printable PDF
Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Send this form to your human resources office. Prior authorization criteria is available. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web medicare advantage prior authorization request form instructions:
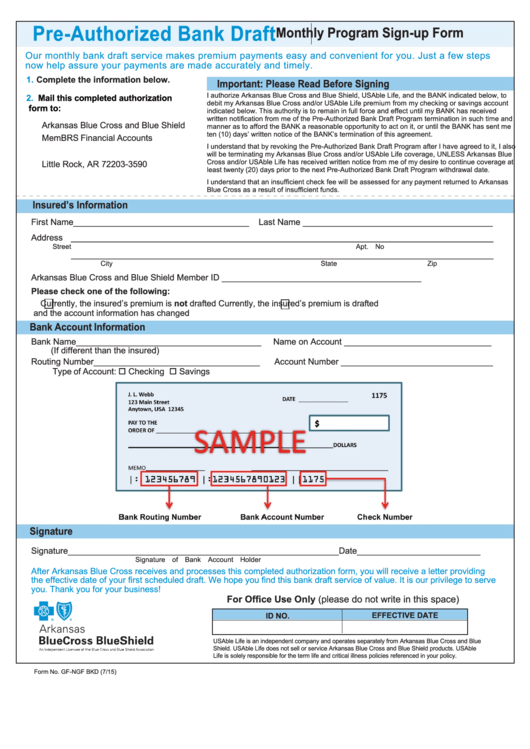
PreAuthorized Bank Draft Arkansas Blue Cross And Blue Shield
Approval information for radiological services Web make changes to existing membership. Annual notice of changes (anocs) For more information about pharmacy prior approval and the required forms visit the prior approval page. Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the.
ASC Coding and Billing Fundamentals Objectives PDF
Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Web prior authorization is a process though which arkansas blue cross and blue shield approves a request for a covered healthcare service before the member receives the. Web make changes to existing membership. Annual notice of changes (anocs) Web please call.
Blue cross blue shield pennsylvania highmark availity
Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the. Approval information for radiological services Web medicare advantage prior authorization request form instructions: Web prior authorization is a process though which arkansas blue cross and blue shield approves a request for a covered healthcare service before the member receives the. Web please call.
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Prior authorization criteria is available. Web select your county on the map below to see plan forms and documents. Web make changes to existing membership. Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the. Web prior approval pharmacy forms.
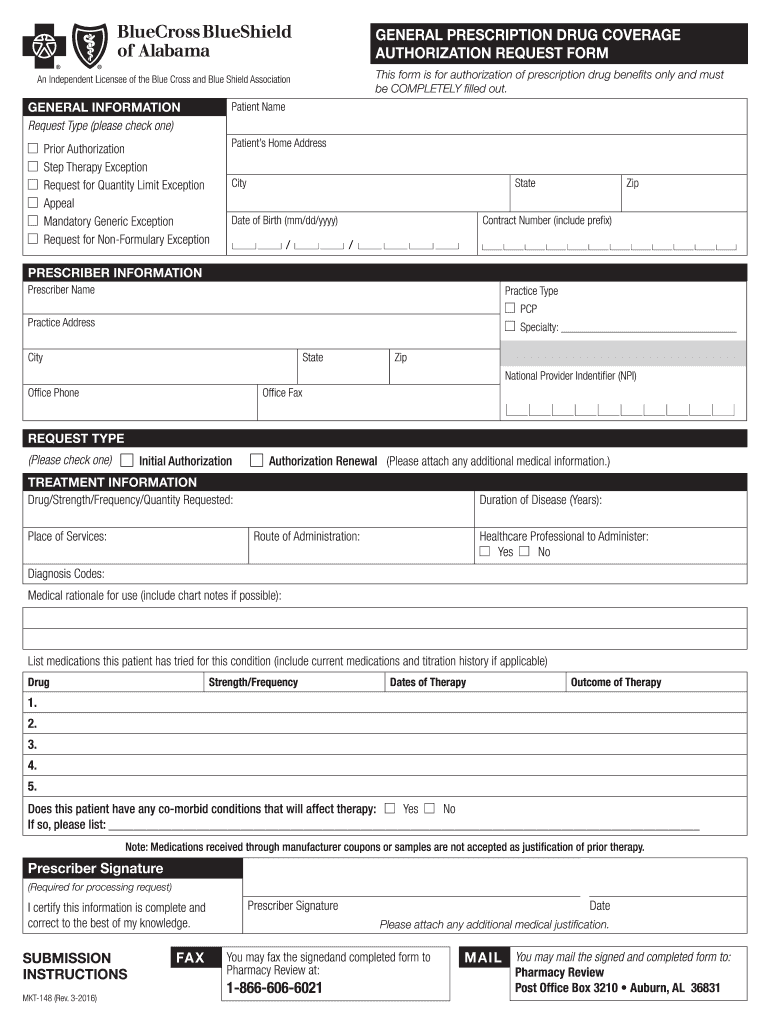
Blue cross blue shield of alabama prior authorization form Fill out
Send this form to your human resources office. Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the. Providers who are requesting a prior approval. Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Approval information for radiological services
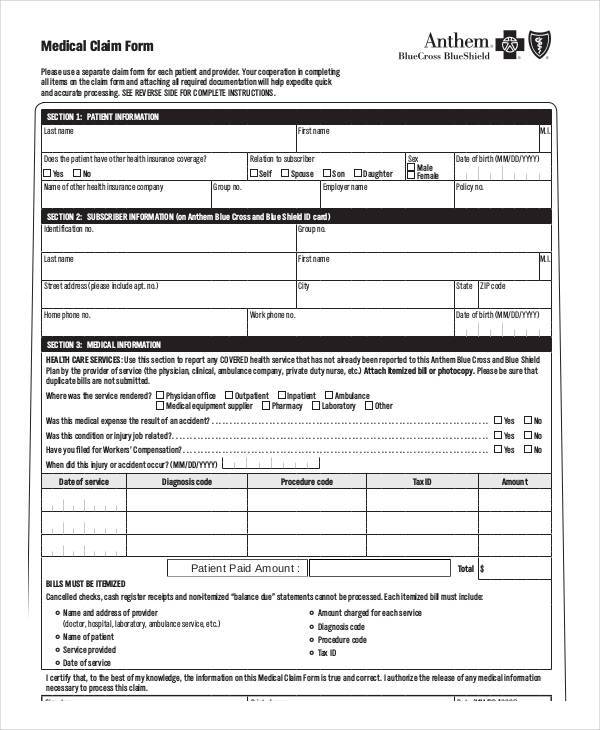
FREE 37+ Blank Medical Forms in PDF MS Word Excel
Arkansas blue cross and blue shield. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web prior approval pharmacy forms. Send this form to your human resources office. Providers who are requesting a prior approval.
Molina Prior Authorization Request Form Fill Online
Web we can help. Web make changes to existing membership. Review the prior authorizations section of the provider manual. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval.
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website. Send this form to your human resources office. Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the. For more information about pharmacy prior approval and the required forms visit the prior approval page..
For More Information About Pharmacy Prior Approval And The Required Forms Visit The Prior Approval Page.
Web select your county on the map below to see plan forms and documents. Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Arkansas blue cross and blue shield. Web providers requesting prior approval for an ase/pse member should use the appropriate form on the health advantage website.
Annual Notice Of Changes (Anocs)
Send this form to your human resources office. Web medicare advantage prior authorization request form instructions: Please fill out all applicable sections on both pages completely and legibly before faxing or mailing the. Prior authorization criteria is available.
Web Prior Approval Pharmacy Forms.
Web make changes to existing membership. Web prior authorization is a process though which arkansas blue cross and blue shield approves a request for a covered healthcare service before the member receives the. Approval information for radiological services Providers who are requesting a prior approval.
Web Please Call Us At 800.753.2851 To Submit A Verbal Prior Authorization Request If You Are Unable To Use Electronic Prior Authorization.
Review the prior authorizations section of the provider manual. Web we can help.