Bcbsil Appeal Form
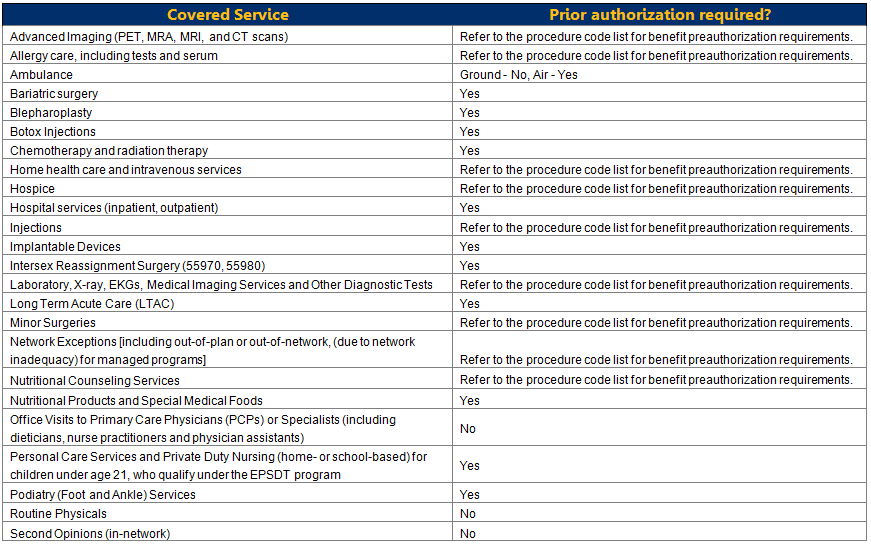
Bcbsil Appeal Form - There are two ways to file an appeal or grievance (complaint): Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. Most provider appeal requests are related to a length of stay or treatment setting denial. If you do not speak english, we can provide an interpreter at no cost to you. By mail or by fax: You may file an appeal in writing by sending a letter or fax: Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Fill out the form below, using the tab key to advance from field to field 2. Web corrected claim review form available on our website at bcbsil.com/provider. When applicable, the dispute option is available in the.
You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. Web this form is for all providers requesting information about claims status or disputing a claim with blue cross and blue shield of illinois (bcbsil) and serving members in the state of illinois. Most provider appeal requests are related to a length of stay or treatment setting denial. Please check “adverse benefit determination” in your benefit booklet for instructions. Include medical records, office notes and any other necessary documentation to support your request 4. Blue cross medicare advantage c/o appeals p.o. Print out your completed form and use it as your cover sheet 3. Most provider appeal requests are related to a length of stay or treatment setting denial. This is different from the request for claim review request process outlined above. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area.
Web this form is for all providers requesting information about claims status or disputing a claim with blue cross and blue shield of illinois (bcbsil) and serving members in the state of illinois. Web how to file an appeal or grievance: By mail or by fax: If you are hearing impaired, call. If you do not speak english, we can provide an interpreter at no cost to you. Web corrected claim review form available on our website at bcbsil.com/provider. Print out your completed form and use it as your cover sheet 3. Fill out the form below, using the tab key to advance from field to field 2. You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. Box 663099 dallas, tx 75266.
BCBSIL (BCBSIL) Twitter
Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. You may file an appeal in writing by sending a letter.
BCBSIL E/M Claim Appeal Template Language Illinois Chiropractic Society
Most provider appeal requests are related to a length of stay or treatment setting denial. You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. You may file an appeal in writing by sending a letter or fax: Print out your completed form and use it.
BCBS Enhanced Certificate
Please check “adverse benefit determination” in your benefit booklet for instructions. Web corrected claim review form available on our website at bcbsil.com/provider. Claim review (medicare advantage ppo) credentialing/contracting. There are two ways to file an appeal or grievance (complaint): Web how to file an appeal or grievance:
BCBSIL Android Apps on Google Play
Web blue cross and blue shield of illinois (bcbsil) has an internal claims and appeals process that allows you to appeal decisions about paying claims, eligibility for coverage or ending coverage. This is different from the request for claim review request process outlined above. You can ask for an appeal if coverage or payment for an item or medical service.
BCBSIL Issues 2019 Medicaid and Medicare Advantage Benefit Pre and
Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. If you do not speak english, we can provide an interpreter at no cost to you. Print out your completed form and use it as your cover sheet 3. Please check “adverse benefit determination” in your benefit booklet for.
BCBSIL (BCBSIL) Twitter
Most provider appeal requests are related to a length of stay or treatment setting denial. Web how to file an appeal or grievance: Claim review (medicare advantage ppo) credentialing/contracting. Most provider appeal requests are related to a length of stay or treatment setting denial. There are two ways to file an appeal or grievance (complaint):
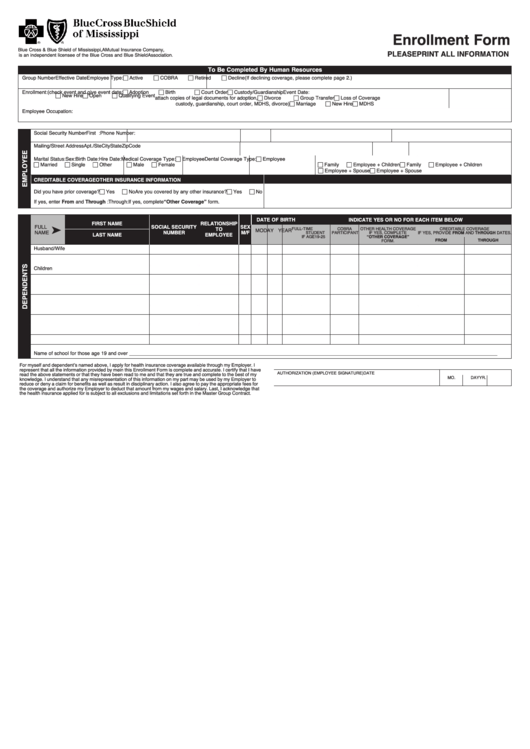
Form Bcbs 16628 Enrollment Form printable pdf download
This is different from the request for claim review request process outlined above. Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. When applicable, the dispute option is available in the. Web a provider appeal is an official request for reconsideration.
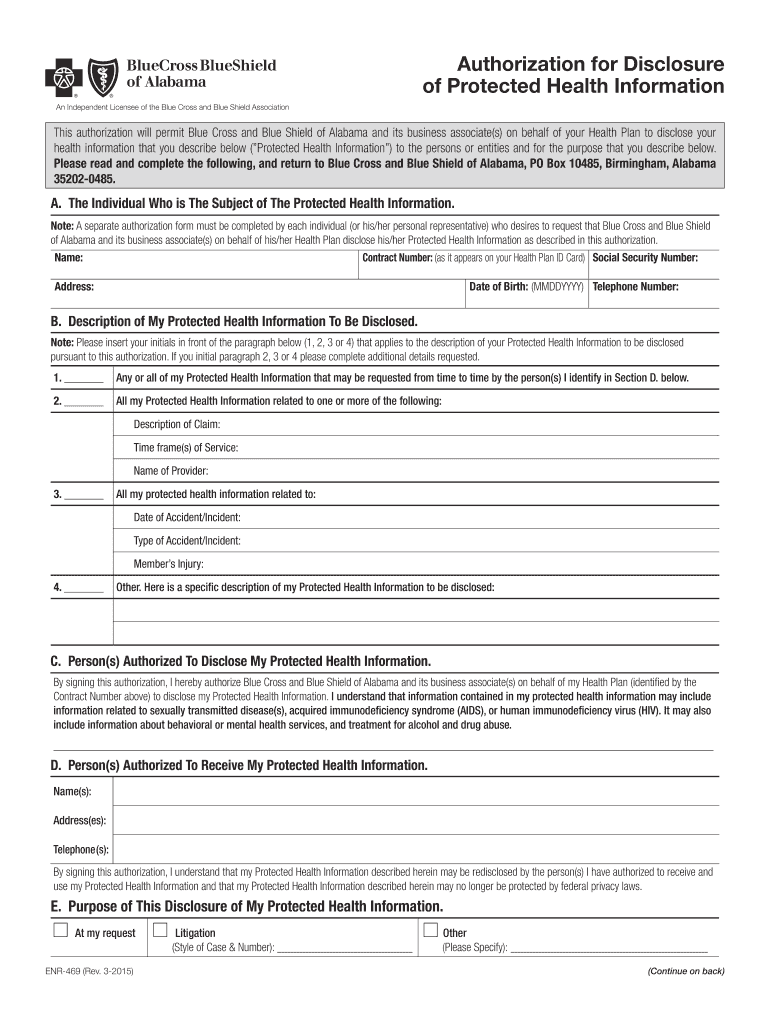
20152022 AL BCBS Form ENR469 Fill Online, Printable, Fillable, Blank
Web blue cross and blue shield of illinois (bcbsil) has an internal claims and appeals process that allows you to appeal decisions about paying claims, eligibility for coverage or ending coverage. You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. If you are hearing impaired,.
BCBSIL (BCBSIL) Twitter
When applicable, the dispute option is available in the. Please check “adverse benefit determination” in your benefit booklet for instructions. By mail or by fax: Claim review (medicare advantage ppo) credentialing/contracting. To submit claim review requests online utilize the claim inquiry resolution tool, accessible through electronic refund management (erm) on the availity ® provider portal at availity.com.
Make a Payment Smith and Associates Inc
To submit claim review requests online utilize the claim inquiry resolution tool, accessible through electronic refund management (erm) on the availity ® provider portal at availity.com. Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. Web blue cross and blue shield.
Web Blue Cross And Blue Shield Of Illinois (Bcbsil) Has An Internal Claims And Appeals Process That Allows You To Appeal Decisions About Paying Claims, Eligibility For Coverage Or Ending Coverage.
Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. You may file an appeal in writing by sending a letter or fax: Claim review (medicare advantage ppo) credentialing/contracting. Web corrected claim review form available on our website at bcbsil.com/provider.
Blue Cross Medicare Advantage C/O Appeals P.o.
By mail or by fax: Include medical records, office notes and any other necessary documentation to support your request 4. Box 663099 dallas, tx 75266. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area.
There Are Two Ways To File An Appeal Or Grievance (Complaint):
You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. To submit claim review requests online utilize the claim inquiry resolution tool, accessible through electronic refund management (erm) on the availity ® provider portal at availity.com. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. If you are hearing impaired, call.
Web This Form Is For All Providers Requesting Information About Claims Status Or Disputing A Claim With Blue Cross And Blue Shield Of Illinois (Bcbsil) And Serving Members In The State Of Illinois.
Web how to file an appeal or grievance: This is different from the request for claim review request process outlined above. If you do not speak english, we can provide an interpreter at no cost to you. Most provider appeal requests are related to a length of stay or treatment setting denial.