Elixir Prior Authorization Form
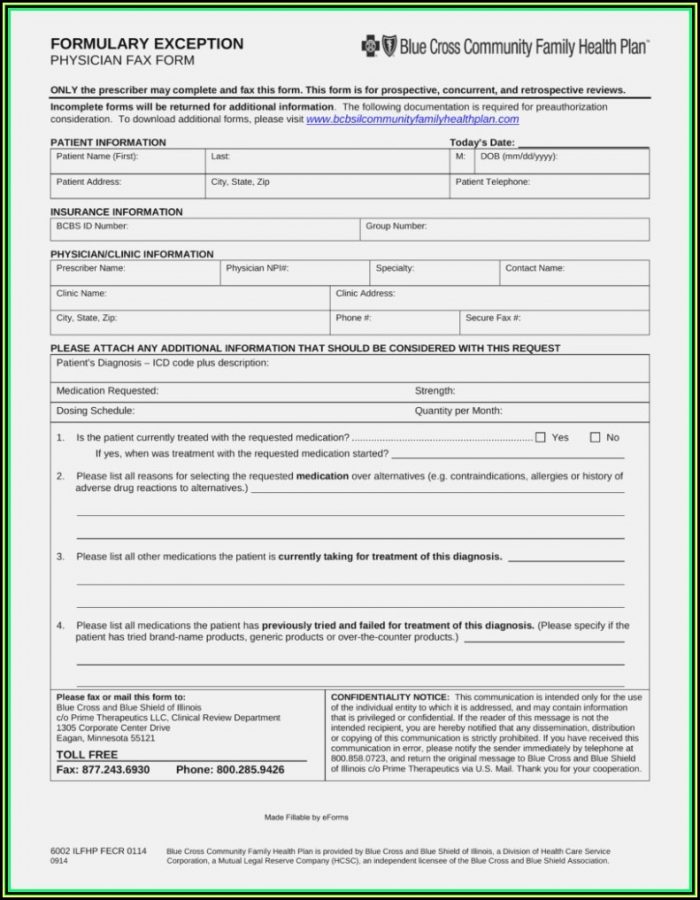
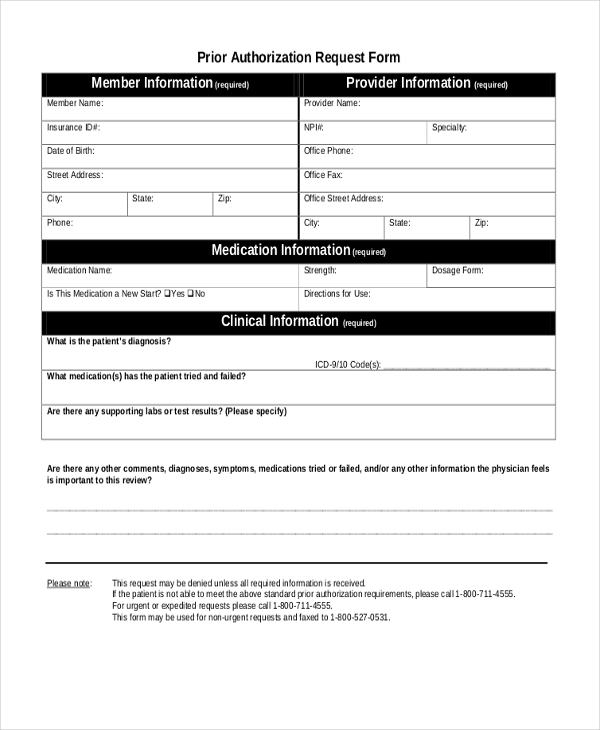
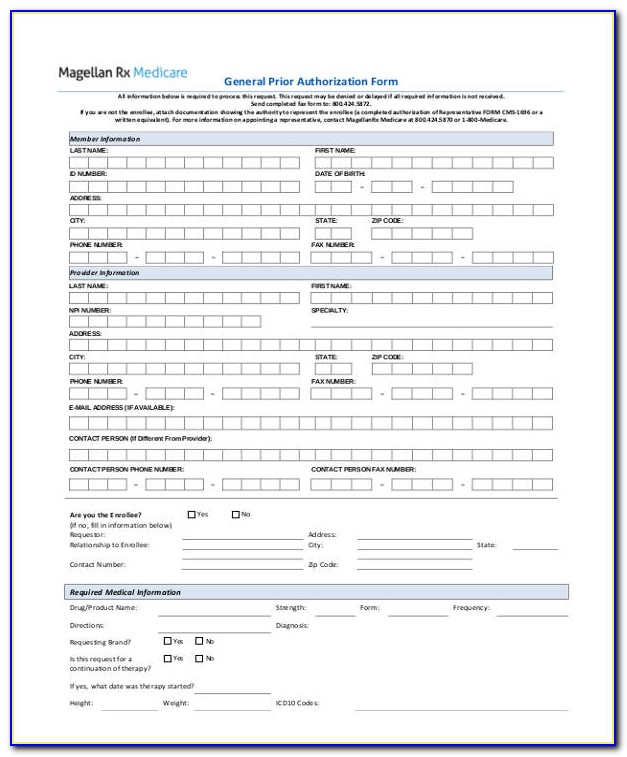
Elixir Prior Authorization Form - Web prior authorization request form. Web coverage determination request form. Web elixir manages the pharmacy drug benefit for your patient. Please answerthe following questions and fax this form to the number listed above. Certain requests for coverage require review with the prescribing physician. Standard (up to 14 days for services/72 hrs. Please note any information left blank or illegible may delay the reviewprocess. Please answer the following questions and fax this form to the number listed above. Covermymeds is elixir solutions' prior authorization forms’s preferred method for receiving epa requests. You can appoint a representative to act on your behalf for filing a coverage determination or appeal by providing us with a completed appointment of representative form or visit the cms medicare website at www.cms.hhs.gov.
Please answer the following questions and fax this form to the. Please answerthe following questions and fax this form to the number listed above. If the prescribed medication requires a prior authorization, you can request a coverage determination request” asking the plan to review the request to approve coverage of the medication. Certain requests for coverage require review with the prescribing physician. Elixir manages the pharmacy drug benefit for your patient. Web coverage determination request form. Please answer the following questions and fax this form to the number listed above. Covermymeds is elixir solutions' prior authorization forms’s preferred method for receiving epa requests. Please note any information left blank or illegible may delay the reviewprocess. Web prior authorization request form.
You can appoint a representative to act on your behalf for filing a coverage determination or appeal by providing us with a completed appointment of representative form or visit the cms medicare website at www.cms.hhs.gov. Please note any information left blank or illegible may delay the reviewprocess. Click here for the promptpa web portal; If the prescribed medication requires a prior authorization, you can request a coverage determination request” asking the plan to review the request to approve coverage of the medication. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Elixir manages the pharmacy drug benefit for your patient. Web medicare prior authorization request phone: Web to find out if your medication requires a prior authorization and to download necessary forms, search the formulary. Elixir manages the pharmacy drug benefit for your patient. Web select the appropriate elixir form to get started.
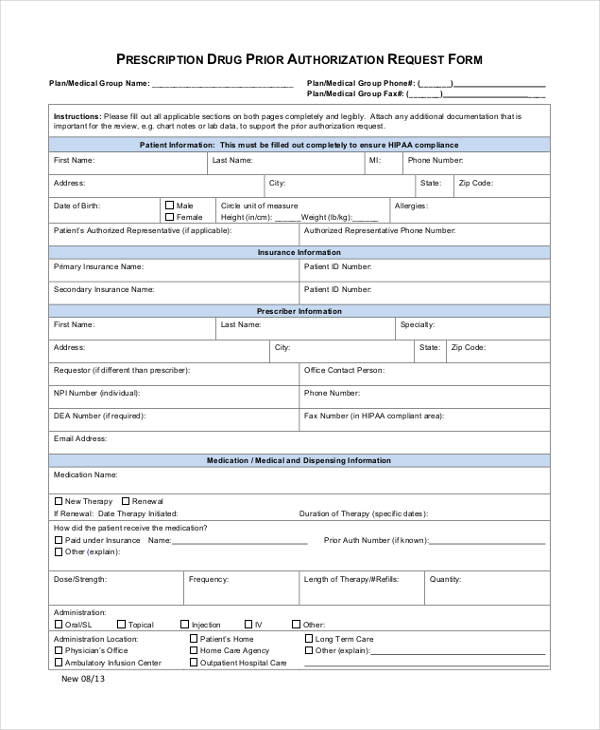
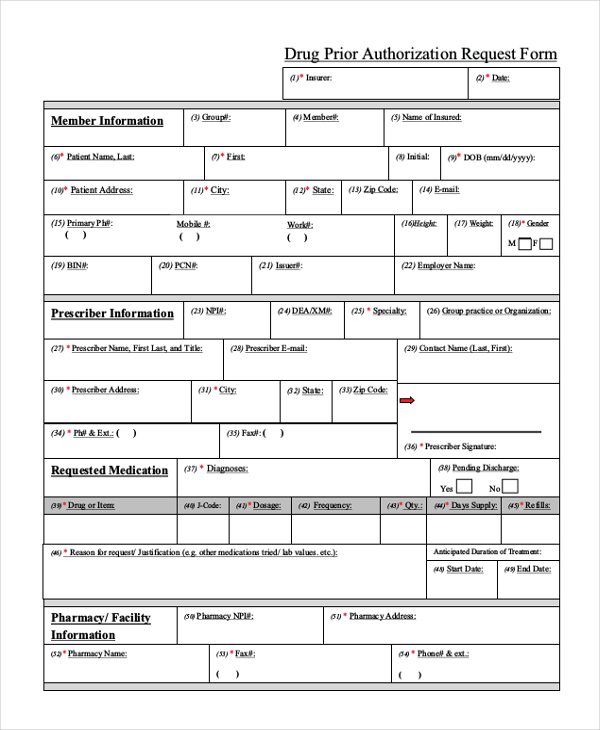
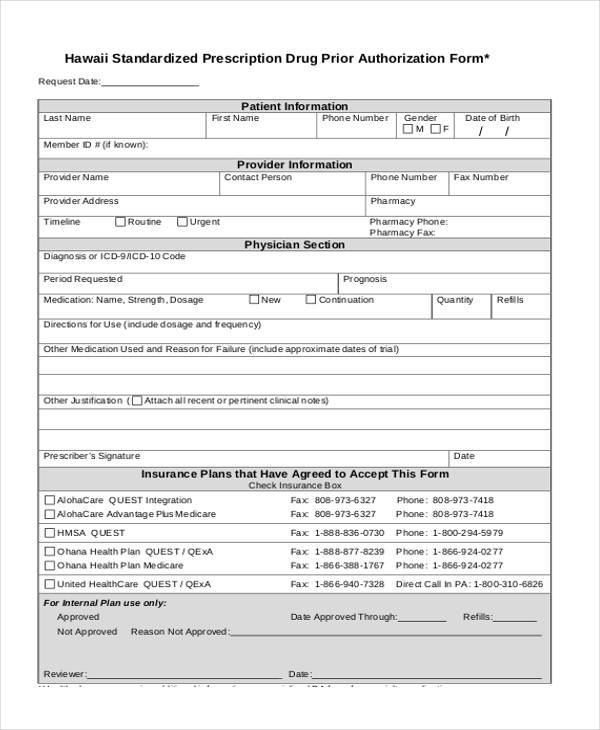
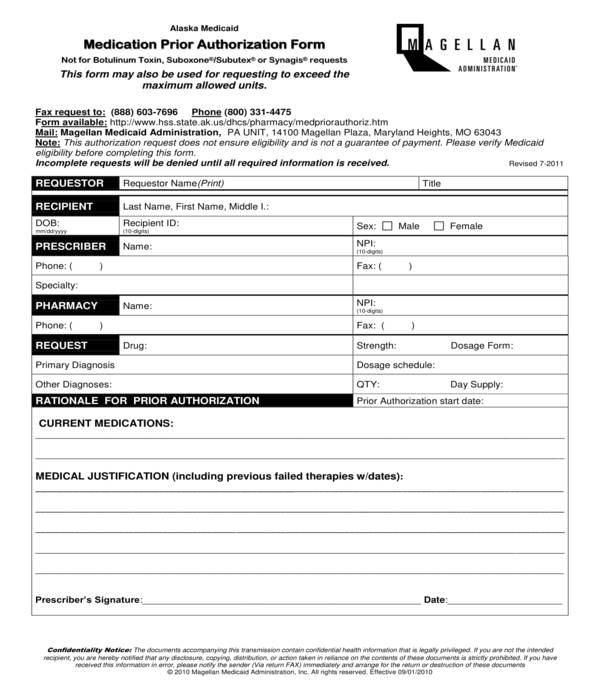
FREE 13+ Prior Authorization Forms in PDF MS Word
Elixir manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the. Part b drugs administered at home, such as insulin, should be directed. Description of service start date of service end date of service service code if available (hcpcs/cpt) new prior.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the. Name of prescription drug you are requesting (if known, include strength and. Web elixir manages the pharmacy drug benefit for your patient. Elixir manages the pharmacy drug benefit for your patient.
FREE 41+ Authorization Forms in PDF Excel MS word
Web coverage determination request form. Within the portal, select the prescriber link to begin Certain requests for coverage require review with the prescribing physician. Web elixir manages the pharmacy drug benefit for your patient. Web to find out if your medication requires a prior authorization and to download necessary forms, search the formulary.
Elixir Met Form Aluk Hyderabad Aluminium Windows & Doors
Web elixir manages the pharmacy drug benefit for your patient. Please answer the following questions and fax this form to the. Web prior authorization request form. If the prescribed medication requires a prior authorization, you can request a coverage determination request” asking the plan to review the request to approve coverage of the medication. Certain requests for coverage require review.
FREE 11+ Prior Authorization Forms in PDF MS Word
Elixir manages the pharmacy drug benefit for your patient. Web prior authorization request form. Web medicare prior authorization request phone: Web to find out if your medication requires a prior authorization and to download necessary forms, search the formulary. Part b drugs administered at home, such as insulin, should be directed.
United Healthcare Medicare Prior Authorization Form Forms NDkyMA
Web to find out if your medication requires a prior authorization and to download necessary forms, search the formulary. Covermymeds is elixir solutions' prior authorization forms’s preferred method for receiving epa requests. Web medicare prior authorization request phone: Description of service start date of service end date of service service code if available (hcpcs/cpt) new prior authorization check status complete.
Sample Ach Deposit Authorization Form Form Resume Examples AjYdnEZ2l0
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Description of service start date of service end date of service service code if available (hcpcs/cpt) new prior authorization check status complete existing request member prescriber pharmacy If the prescribed medication requires a prior authorization, you can request a.
FREE 10+ Sample Medicare Forms in PDF MS Word
Web elixir manages the pharmacy drug benefit for your patient. To submit a prior authorization request: Certain requests for coverage require review with the prescribing physician. Part b drugs administered at home, such as insulin, should be directed. Please note any information left blank or illegible may delay the reviewprocess.
Amerigroup Medicare Advantage Prior Authorization Forms Form Resume
Web select the appropriate elixir form to get started. Description of service start date of service end date of service service code if available (hcpcs/cpt) new prior authorization check status complete existing request member prescriber pharmacy To submit a prior authorization request: Standard (up to 14 days for services/72 hrs. Certain requests for coverage require review with the prescribing physician.
Elixir LinkedIn
Please answer the following questions and fax this form to the number listed above. If the prescribed medication requires a prior authorization, you can request a coverage determination request” asking the plan to review the request to approve coverage of the medication. To submit a prior authorization request: Please answerthe following questions and fax this form to the number listed.
Description Of Service Start Date Of Service End Date Of Service Service Code If Available (Hcpcs/Cpt) New Prior Authorization Check Status Complete Existing Request Member Prescriber Pharmacy
Web to find out if your medication requires a prior authorization and to download necessary forms, search the formulary. Part b drugs administered at home, such as insulin, should be directed. Standard (up to 14 days for services/72 hrs. Web coverage determination request form.
Within The Portal, Select The Prescriber Link To Begin
Elixir manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Name of prescription drug you are requesting (if known, include strength and. Web elixir manages the pharmacy drug benefit for your patient.
Web Coverage Determination Request Form.
Elixir manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Web prior authorization request form. If the prescribed medication requires a prior authorization, you can request a coverage determination request” asking the plan to review the request to approve coverage of the medication.
Web Select The Appropriate Elixir Form To Get Started.
Please answer the following questions and fax this form to the. Please note any information left blank or illegible may delay the reviewprocess. Click here for the promptpa web portal; You can appoint a representative to act on your behalf for filing a coverage determination or appeal by providing us with a completed appointment of representative form or visit the cms medicare website at www.cms.hhs.gov.