Express Scripts Appeal Form
Express Scripts Appeal Form - The medical staff will need to fill out the form with the patient’s personal and medical details, as well the prescriber’s. Representation documentation for requests made by someone other than the enrollee or the enrollee's prescriber: An express scripts prior authorization form is meant to be used by medical offices when requesting coverage for a patient’s prescription. Web express scripts prior (rx) authorization form. Web include a copy of the claim decision, and. Web follow these steps to get your express scripts appeal edited for the perfect workflow: You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Select the get form button on this page. Web download pdf online application to submit a redetermination request form if you would like to request a coverage determination (such as an exception to the rules or restriction on our plan's coverage of a drug) or if you would like to make an appeal for us to reconsider a coverage decision, you may: Web to initiate a coverage review request, please complete the form below and click submit.
You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Web include a copy of the claim decision, and. Web all you need to do is to pick the express scripts prior authorization, fill out the appropriate document parts, drag and drop fillable fields (if necessary), and certify it without having second guessing about whether or not your signed document is legally binding. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: How to shield your express scripts claims form when doing it online? Representation documentation for requests made by someone other than the enrollee or the enrollee's prescriber: Web since your request for coverage of (or payment for) a prescription drug was denied, you have the right to ask us for a redetermination (appeal) of our decision. This form may be sent to us by mail or fax: Web to initiate a coverage review request, please complete the form below and click submit. Web express scripts prior (rx) authorization form.
Web download pdf online application to submit a redetermination request form if you would like to request a coverage determination (such as an exception to the rules or restriction on our plan's coverage of a drug) or if you would like to make an appeal for us to reconsider a coverage decision, you may: If you request an exception, your doctor must provide a statement to support your request. Web all you need to do is to pick the express scripts prior authorization, fill out the appropriate document parts, drag and drop fillable fields (if necessary), and certify it without having second guessing about whether or not your signed document is legally binding. Representation documentation for requests made by someone other than the enrollee or the enrollee's prescriber: The medical staff will need to fill out the form with the patient’s personal and medical details, as well the prescriber’s. Web individual request electronic phi third party request for electronic protected health information to make a bulk request for electronic data, please download this form. Web since your request for coverage of (or payment for) a prescription drug was denied, you have the right to ask us for a redetermination (appeal) of our decision. Web express scripts prior (rx) authorization form. Enrollee/requestor information complete this section only if the person making this request is not the enrollee or prescriber: Web include a copy of the claim decision, and.
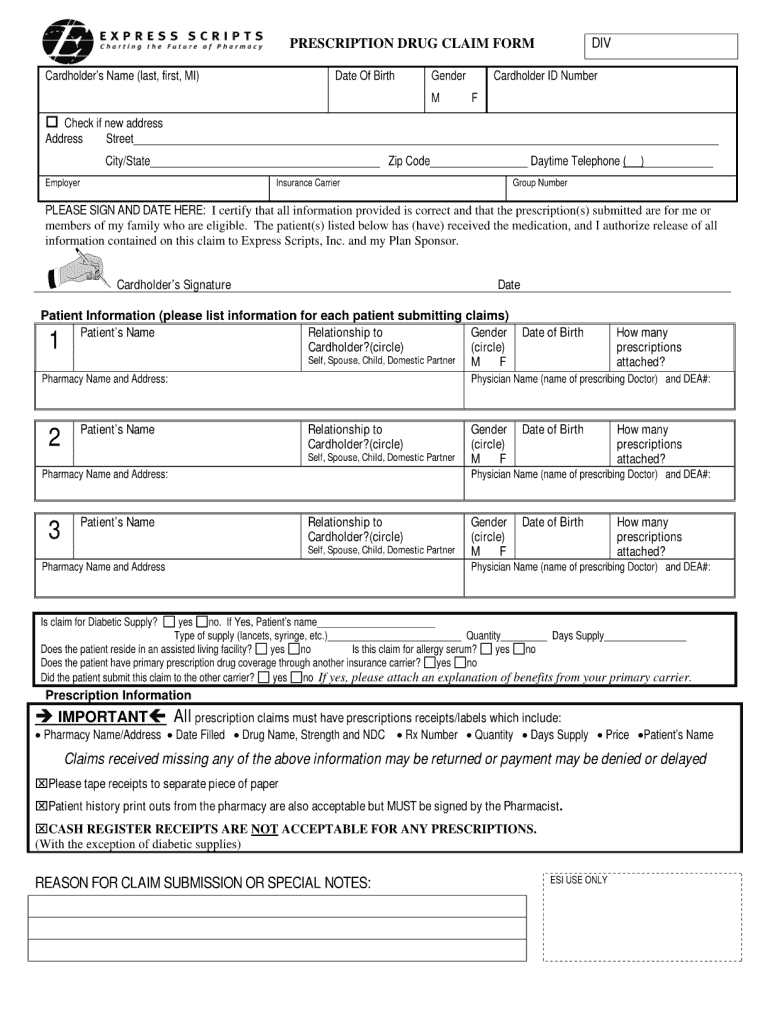
Free Express Scripts Prior (Rx) Authorization Form PDF eForms
An express scripts prior authorization form is meant to be used by medical offices when requesting coverage for a patient’s prescription. Web express scripts prior (rx) authorization form. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: Web individual request electronic phi third party request for electronic protected.
Express Scripts Fax Forms for Physicians Prior Authorization Fill Out
Web download pdf online application to submit a redetermination request form if you would like to request a coverage determination (such as an exception to the rules or restriction on our plan's coverage of a drug) or if you would like to make an appeal for us to reconsider a coverage decision, you may: You have 60 days from the.
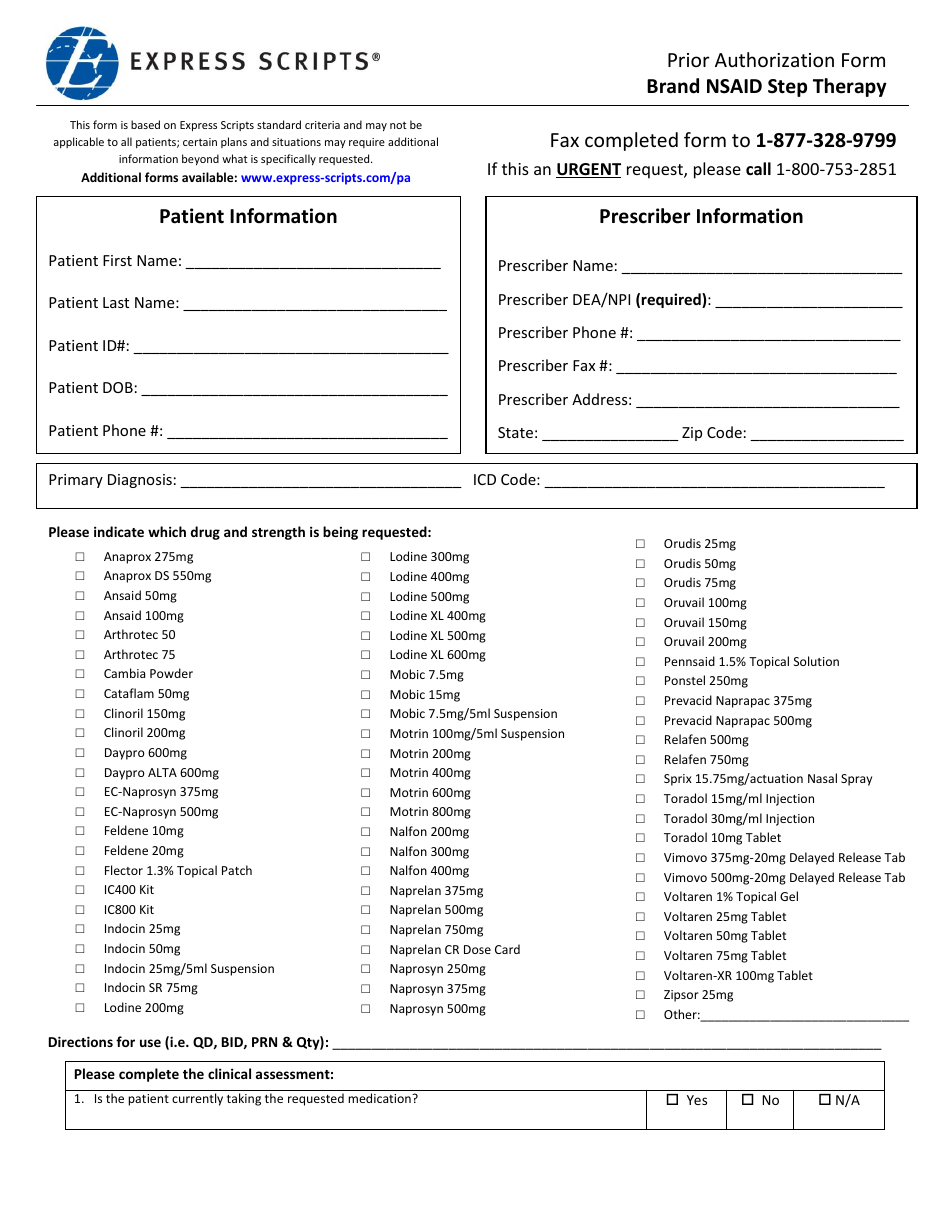
Prior Authorization Form Brand Nsaid Step Therapy Express Scripts
You will enter into our pdf editor. An express scripts prior authorization form is meant to be used by medical offices when requesting coverage for a patient’s prescription. Web download pdf online application to submit a redetermination request form if you would like to request a coverage determination (such as an exception to the rules or restriction on our plan's.
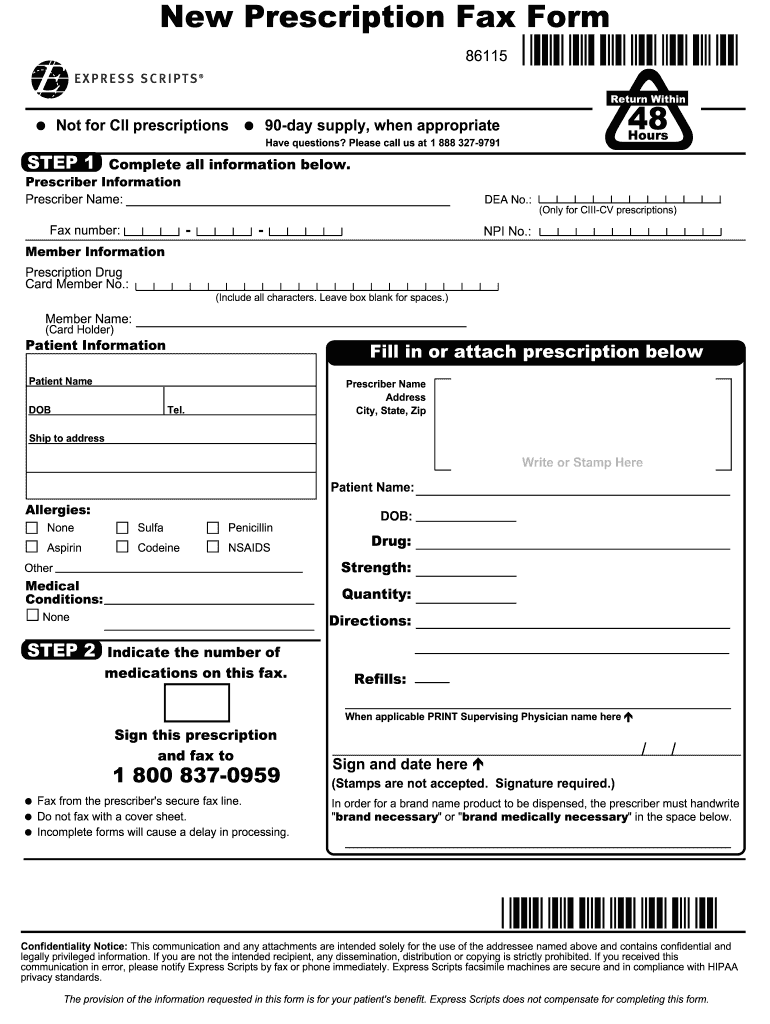
Express Scripts New Prescription Fax Form Fill and Sign Printable
Web to initiate a coverage review request, please complete the form below and click submit. You may submit more documentation to support your appeal. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: An express scripts prior authorization form is meant to be used by medical offices when.
Express Scripts Headquarters and Technology & Innovation Center
Web individual request electronic phi third party request for electronic protected health information to make a bulk request for electronic data, please download this form. How to shield your express scripts claims form when doing it online? An express scripts prior authorization form is meant to be used by medical offices when requesting coverage for a patient’s prescription. Web all.
57 HQ Images Express Scripts Appeal Form Express Scripts Prior
Web follow these steps to get your express scripts appeal edited for the perfect workflow: How to shield your express scripts claims form when doing it online? Web individual request electronic phi third party request for electronic protected health information to make a bulk request for electronic data, please download this form. Web drug, you have the right to ask.
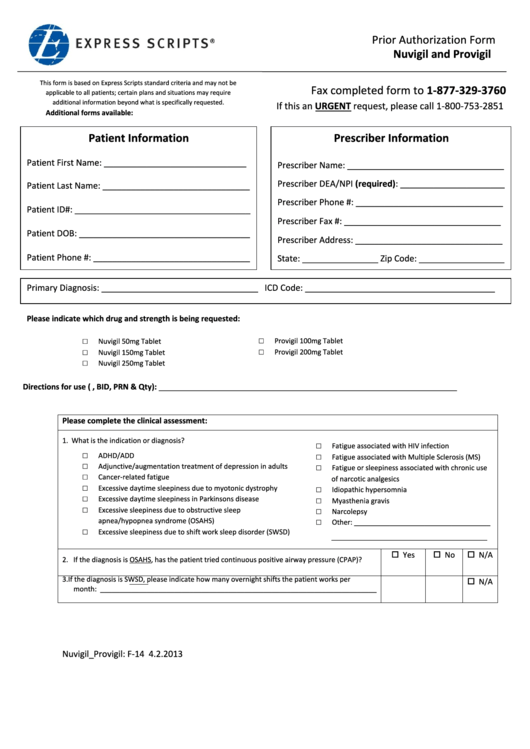
Express Scripts Prior Authorization Form Nuvigil And Provigil
Enrollee/requestor information complete this section only if the person making this request is not the enrollee or prescriber: Web to initiate a coverage review request, please complete the form below and click submit. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: Select the get form button on.
How to Get Prescription Refill Home
This form may be sent to us by mail or fax: You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Representation documentation for requests made by someone other than the enrollee or the enrollee's prescriber: Web to initiate a coverage review request, please complete the form.
57 HQ Images Express Scripts Appeal Form Express Scripts Prior
Web to initiate a coverage review request, please complete the form below and click submit. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: Web drug, you have the right to ask us for a redetermination (appeal) of our decision. This form may be sent to us by.
Express Scripts Appeal Form Fill Online, Printable, Fillable, Blank
Web follow these steps to get your express scripts appeal edited for the perfect workflow: Enrollee/requestor information complete this section only if the person making this request is not the enrollee or prescriber: You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Web all you need.
Web Include A Copy Of The Claim Decision, And.
If you request an exception, your doctor must provide a statement to support your request. You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Web download pdf online application to submit a redetermination request form if you would like to request a coverage determination (such as an exception to the rules or restriction on our plan's coverage of a drug) or if you would like to make an appeal for us to reconsider a coverage decision, you may: Web individual request electronic phi third party request for electronic protected health information to make a bulk request for electronic data, please download this form.
Enrollee/Requestor Information Complete This Section Only If The Person Making This Request Is Not The Enrollee Or Prescriber:
You may submit more documentation to support your appeal. Web to initiate a coverage review request, please complete the form below and click submit. You have 60 days from the date of our notice of denial of medicare prescription drug coverage to ask us for a redetermination. Representation documentation for requests made by someone other than the enrollee or the enrollee's prescriber:
Web Since Your Request For Coverage Of (Or Payment For) A Prescription Drug Was Denied, You Have The Right To Ask Us For A Redetermination (Appeal) Of Our Decision.
Web all you need to do is to pick the express scripts prior authorization, fill out the appropriate document parts, drag and drop fillable fields (if necessary), and certify it without having second guessing about whether or not your signed document is legally binding. You will enter into our pdf editor. Be postmarked or received by express scripts within a deadline of 90 calendar days from the date of the decision to: An express scripts prior authorization form is meant to be used by medical offices when requesting coverage for a patient’s prescription.
How To Shield Your Express Scripts Claims Form When Doing It Online?
The medical staff will need to fill out the form with the patient’s personal and medical details, as well the prescriber’s. Web follow these steps to get your express scripts appeal edited for the perfect workflow: Web express scripts prior (rx) authorization form. Web drug, you have the right to ask us for a redetermination (appeal) of our decision.