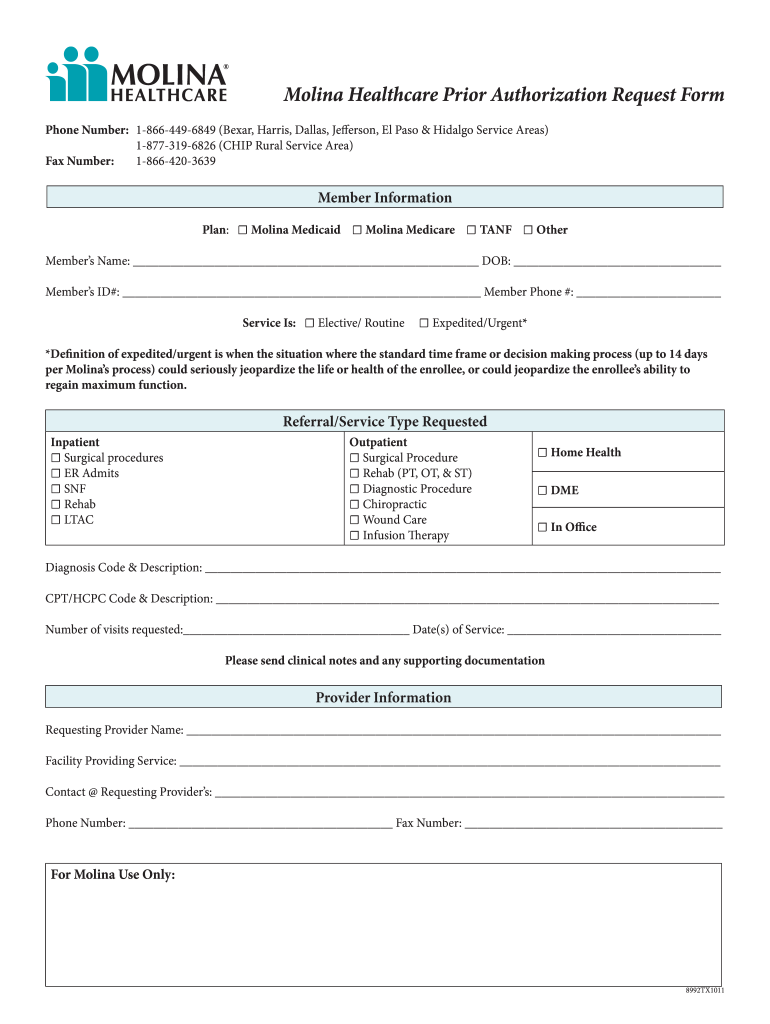
Molina Medicaid Prior Authorization Form
Molina Medicaid Prior Authorization Form - Add or terminate a provider. Items on this list will only be dispensed after prior authorization from molina healthcare. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Change office location, hours, phone, fax, or email. • current (up to 6 months), adequate patient history related to the requested. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. Please click the links below to view documents related to prior authorization requirements. Molina healthcare prior authorization request form and instructions. The forms are also available on the frequently used forms page. It is needed before you can get certain services or drugs.
Add or close a location. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. It is needed before you can get certain services or drugs. Web prior authorization is not a guarantee of payment for services. Medicaid prior authorization annual review report. • current (up to 6 months), adequate patient history related to the requested. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. The forms are also available on the frequently used forms page. Please click the links below to view documents related to prior authorization requirements. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes:
Items on this list will only be dispensed after prior authorization from molina healthcare. Molina healthcare prior authorization request form and instructions. Medicaid prior authorization annual review change log. Please click the links below to view documents related to prior authorization requirements. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Web prior authorization is not a guarantee of payment for services. Add or terminate a provider. Change office location, hours, phone, fax, or email. If prior authorization is needed for a certain service, your provider must get it before giving you the service. Medicaid prior authorization annual review report.
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Molina healthcare prior authorization request form and instructions. Add or close a location. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. It is needed before you can get certain services or drugs. Medicaid prior authorization annual review change log.
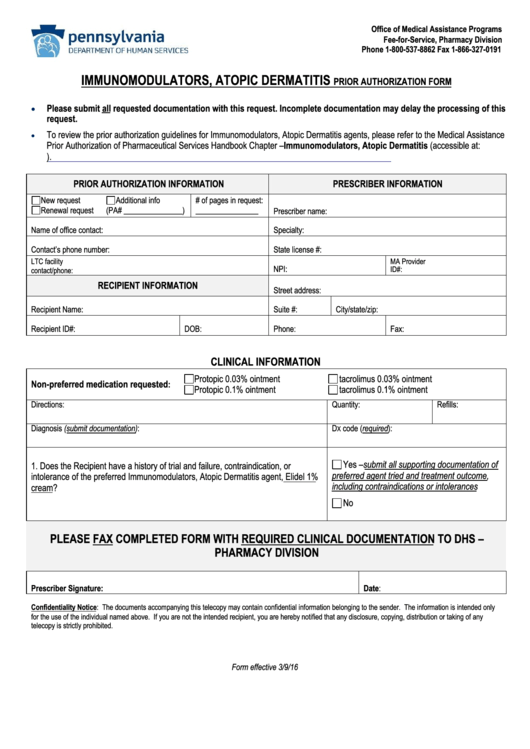
157 Prior Authorization free to download in PDF
Web prior authorization is not a guarantee of payment for services. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. Add or terminate a provider. Items on this list will only be dispensed after prior authorization from molina healthcare. Web all general/physical health prior authorization requests can be submitted via the availity.
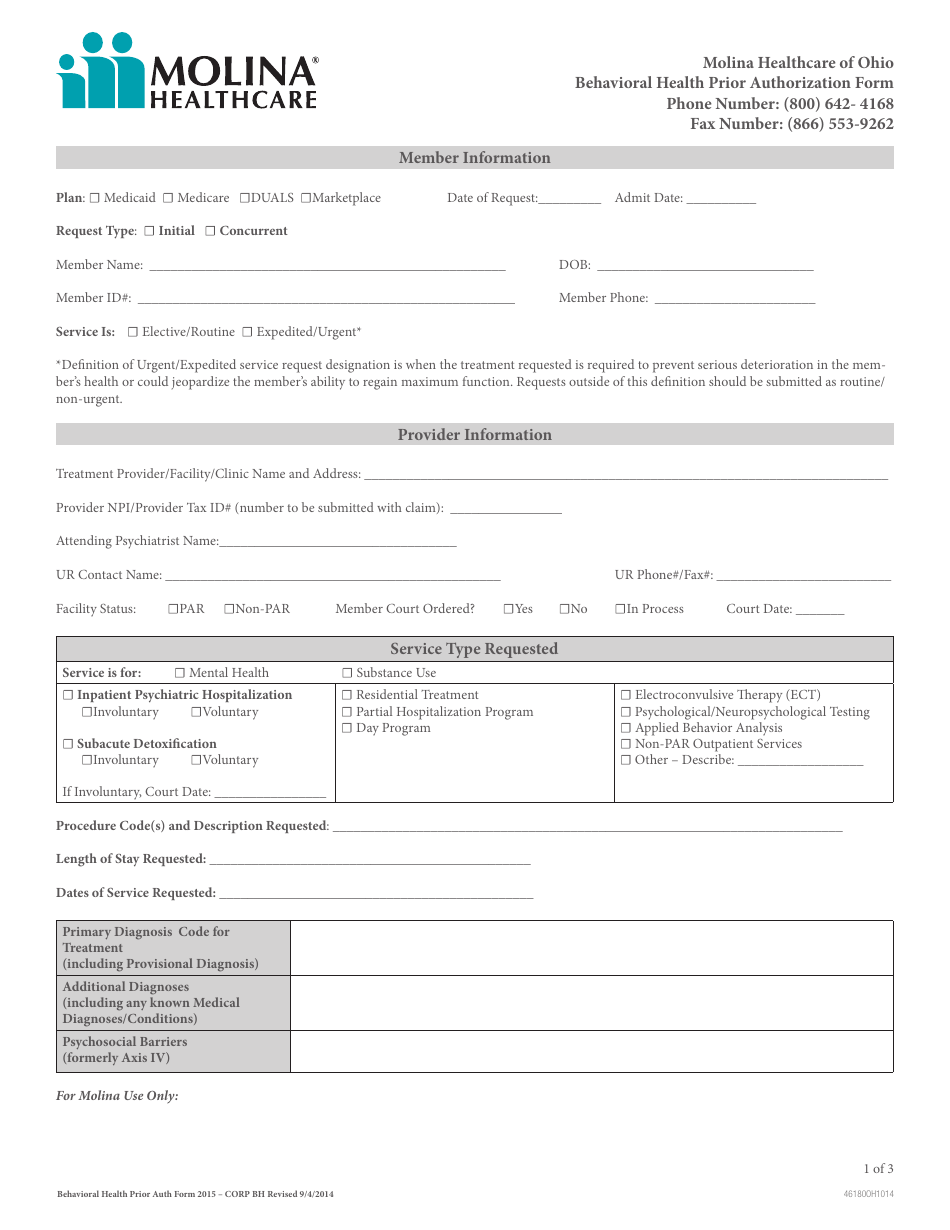
Ohio Behavioral Health Prior Authorization Molina Healthcare Download
Web what are prior authorizations? Items on this list will only be dispensed after prior authorization from molina healthcare. It is needed before you can get certain services or drugs. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: The forms are also available on.
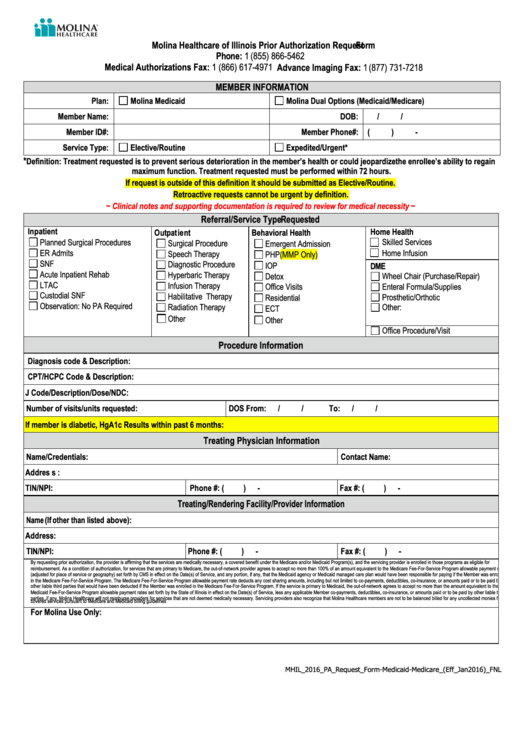
Molina Healthcare Of Illinois Prior Authorization Request printable pdf
Add or terminate a provider. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Molina healthcare prior authorization request form and instructions. The forms are also available on the frequently used forms page. • current (up to 6 months), adequate patient history related to the.
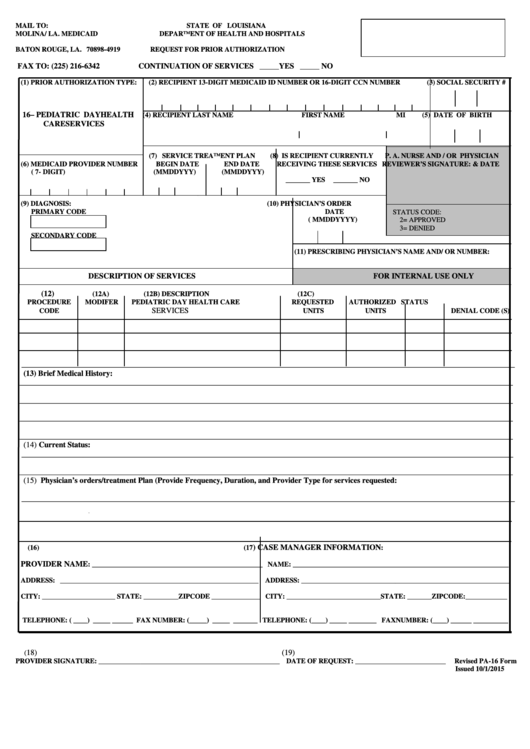
Prior Authorization Form (Pa16) Molina / La. Medicaid printable pdf
Web prior authorization is not a guarantee of payment for services. Molina healthcare prior authorization request form and instructions. The forms are also available on the frequently used forms page. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Molina healthcare prior authorization request form and instructions.
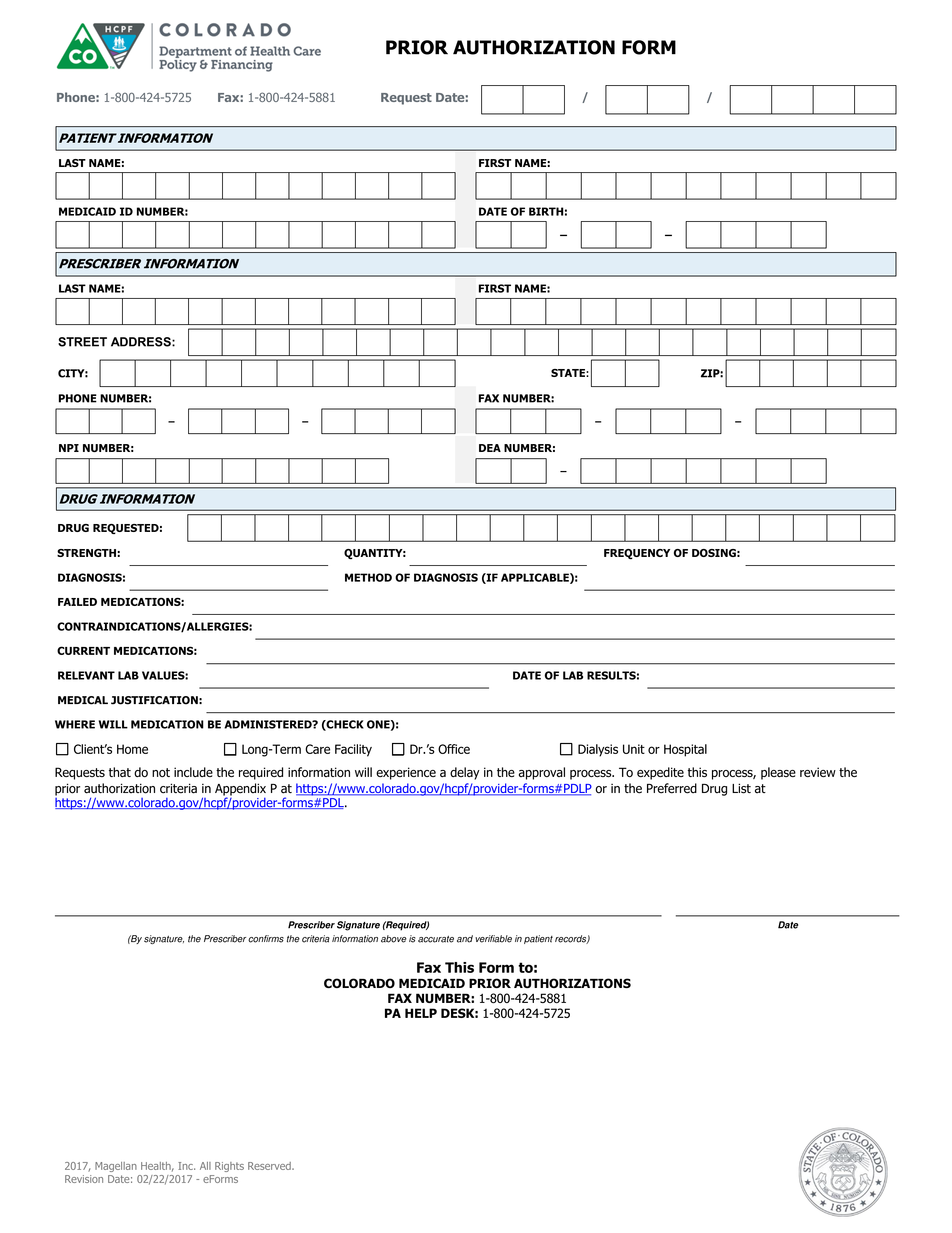
Free Colorado Medicaid Prior (Rx) Authorization Form PDF eForms
Items on this list will only be dispensed after prior authorization from molina healthcare. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. Medicaid prior authorization annual review report. Web what are prior authorizations? • current (up to 6 months), adequate patient history related to the requested.
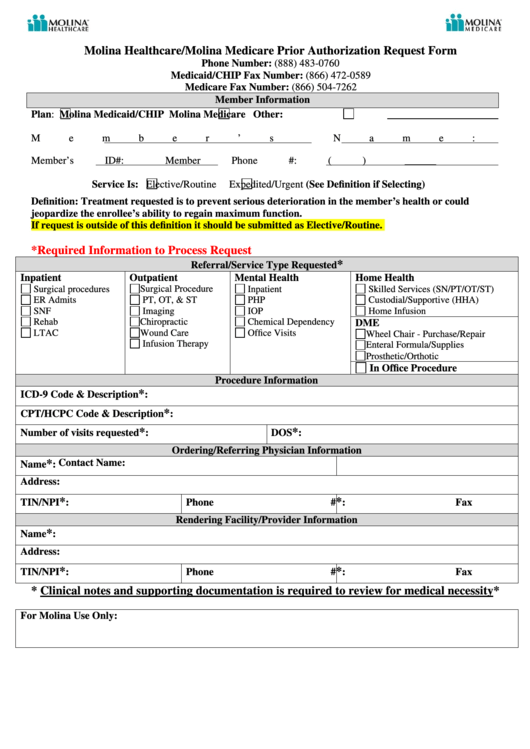
Molina Healthcare/molina Medicare Prior Authorization Request Form
Medicaid prior authorization annual review change log. Medicaid prior authorization annual review report. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Please click the links below to view documents related to prior authorization requirements. Molina healthcare prior authorization request form and instructions.
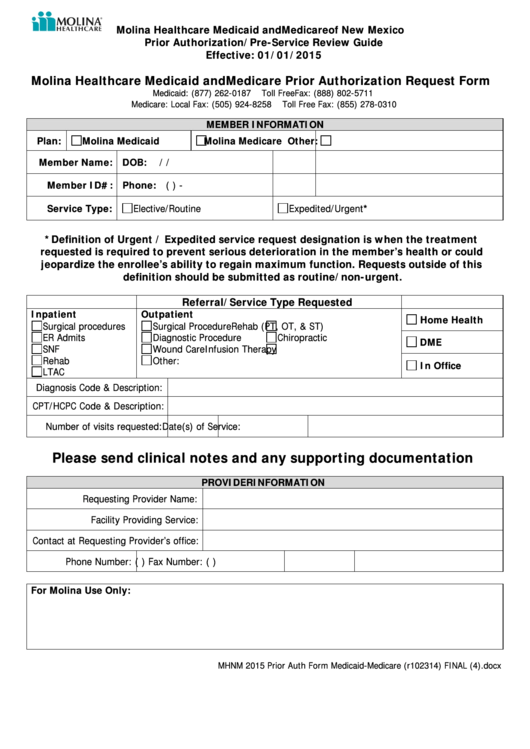
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Medicaid prior authorization annual review report. It is needed before you can get certain services or drugs. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Molina healthcare prior authorization request form and instructions. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
Prior Authorization Washington State Local Health Insurance CHPW
Behavioral health respite services pa reference guide. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. It is needed before you can get certain services or drugs. Items on this list will only be dispensed after prior authorization from molina healthcare. Medicaid prior authorization annual review report.
MOLINA HEALTHCARE, INC. FORM 8K EX99.1 September 16, 2011
If prior authorization is needed for a certain service, your provider must get it before giving you the service. • current (up to 6 months), adequate patient history related to the requested. The forms are also available on the frequently used forms page. It is needed before you can get certain services or drugs. Web we welcome your feedback and.
Please Click The Links Below To View Documents Related To Prior Authorization Requirements.
Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. The forms are also available on the frequently used forms page. If prior authorization is needed for a certain service, your provider must get it before giving you the service.
Add Or Close A Location.
Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Medicaid prior authorization annual review report. Items on this list will only be dispensed after prior authorization from molina healthcare.
Molina Healthcare Prior Authorization Request Form And Instructions.
Web what are prior authorizations? • current (up to 6 months), adequate patient history related to the requested. Molina healthcare prior authorization request form and instructions. Medicaid prior authorization annual review change log.
Behavioral Health Respite Services Pa Reference Guide.
Change office location, hours, phone, fax, or email. It is needed before you can get certain services or drugs. Add or terminate a provider. Web prior authorization is not a guarantee of payment for services.