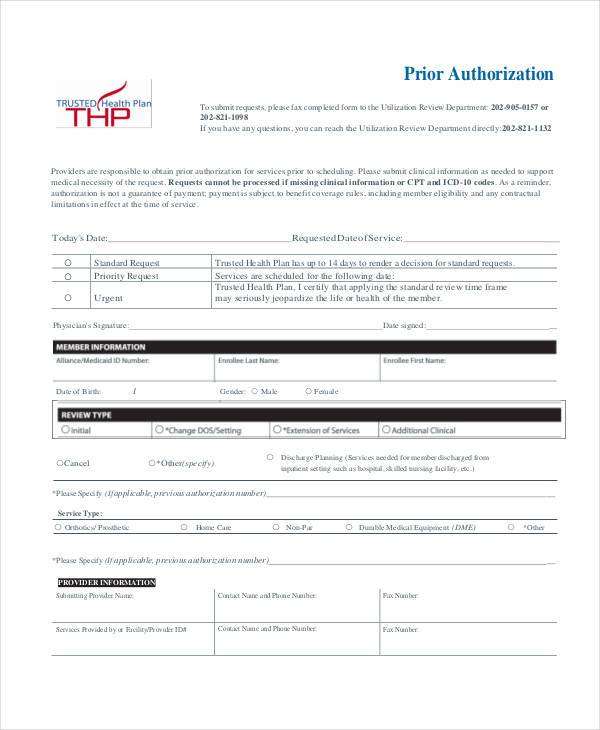
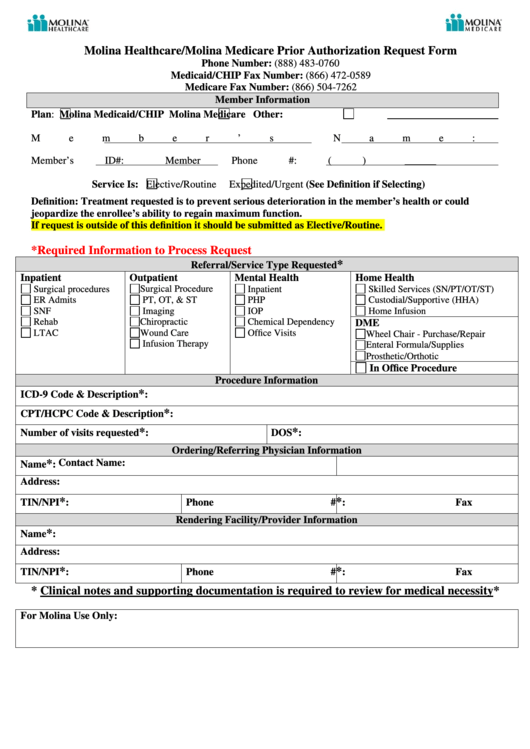
Molina Medicare Prior Authorization Form
Molina Medicare Prior Authorization Form - Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. Web medicaid behavioral health and medical services prior authorization code matrix. Only your provider can request a prior authorization to molina healthcare. Behavioral health service request form. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Web for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologixvia the molina provider portal. Texas standardized prior authorization request form for healthcare services. These tools provide a more efficient, clear process for the submission of. Web o for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologix via the molina provider portal. Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive.
Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare prior authorization forms to the medicare provider page of. Web o for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologix via the molina provider portal. Only your provider can request a prior authorization to molina healthcare. Pharmacy and outpatient drug services. Behavioral health service request form. Texas standardized prior authorization request form for healthcare services. These tools provide a more efficient, clear process for the submission of. Molina healthcare will review the request and let the provider know if the service is approved. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive.
Only your provider can request a prior authorization to molina healthcare. Texas standardized prior authorization request form for healthcare services. Behavioral health service request form. Prior authorization is not a. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. These tools provide a more efficient, clear process for the submission of. Molina healthcare will review the request and let the provider know if the service is approved. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Web medicaid behavioral health and medical services prior authorization code matrix. Pharmacy and outpatient drug services.
Medicare Hospital Stay 3 Days Medicare Prescription Prior
Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. Molina healthcare will review the request and let the provider know if the service is approved. Pharmacy and outpatient drug services..
Molina Medicare Medication Prior Authorization Form Form Resume
Only your provider can request a prior authorization to molina healthcare. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. Web the molina medicare utilization department has posted an updated.
Bcbs Prior Authorization Form Medication Form Resume Examples
Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive. Behavioral health service request form. Pharmacy and outpatient drug services. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health.
Molina Medicare Medication Prior Authorization Form Form Resume
Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare prior authorization forms to the medicare provider page of. Prior authorization is not a. Molina healthcare will review the request and let the provider know if the service is approved. Only your provider can request a prior authorization to molina healthcare. Web.
Molina Medicare Pa Forms Universal Network
Prior authorization is not a. Behavioral health service request form. These tools provide a more efficient, clear process for the submission of. Texas standardized prior authorization request form for healthcare services. Molina healthcare will review the request and let the provider know if the service is approved.
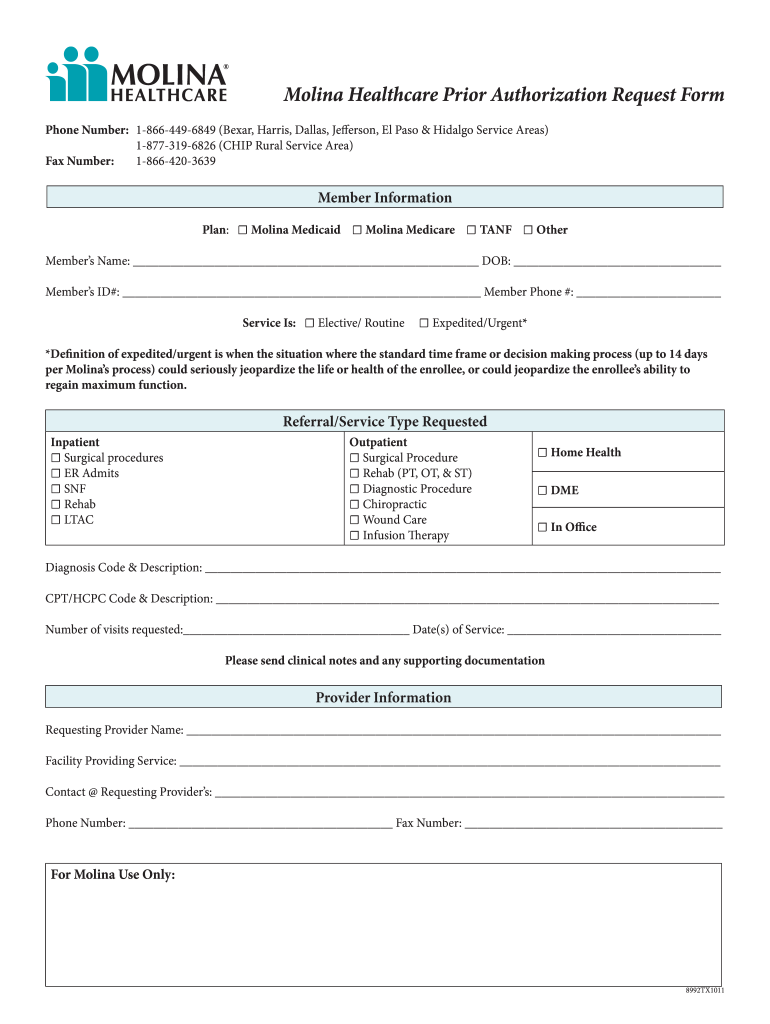
Molina Healthcare/molina Medicare Prior Authorization Request Form
Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive. Web medicaid behavioral health and medical services prior authorization code matrix. These tools provide a more efficient, clear process for the submission of. Texas standardized prior authorization request form for healthcare services. Prior authorization is not a.
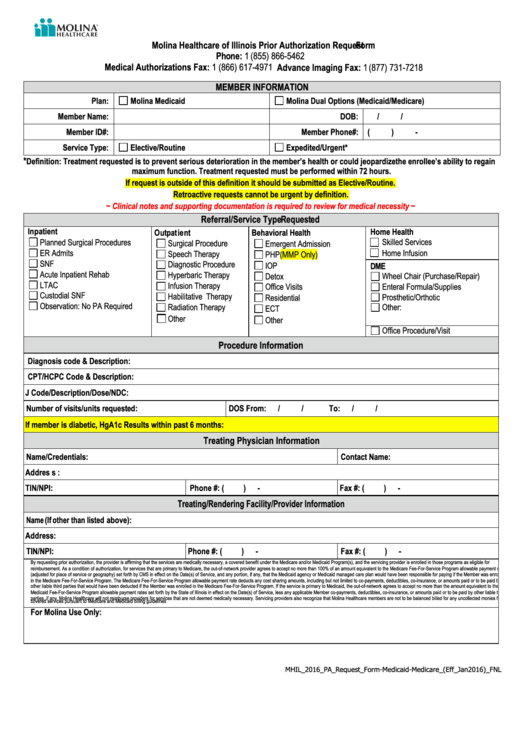
Molina Healthcare Of Illinois Prior Authorization Request printable pdf
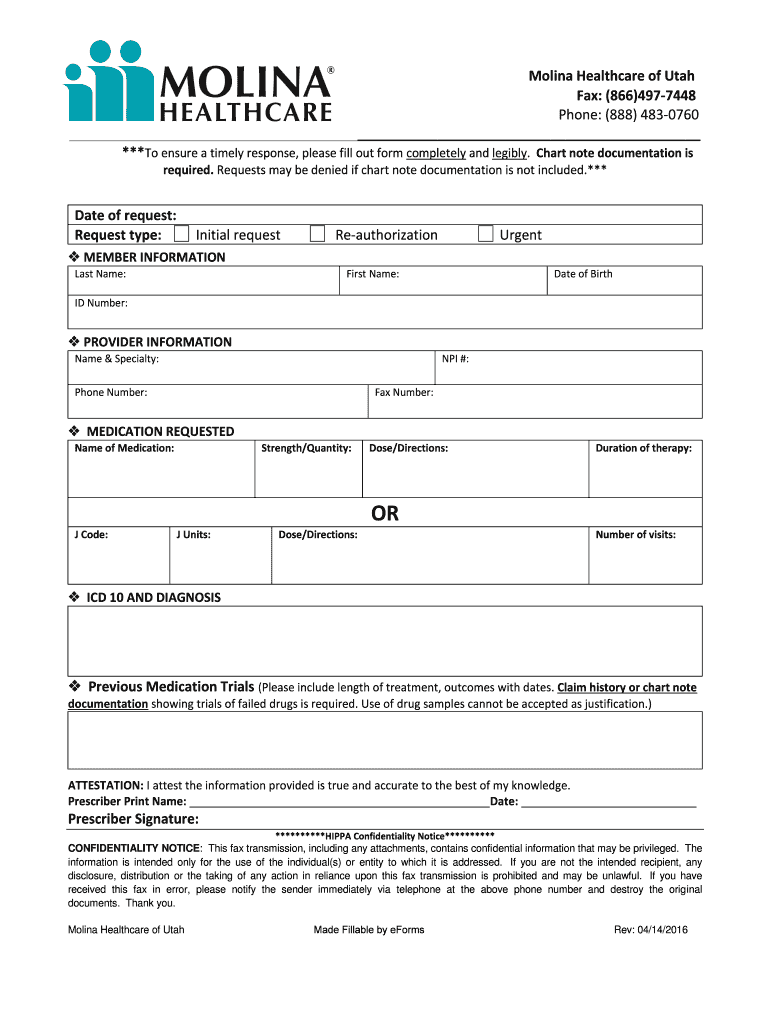
Pharmacy and outpatient drug services. Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare prior authorization forms to the medicare provider page of. Texas standardized prior authorization request form for healthcare services. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Web medicaid behavioral health and medical services prior authorization code.
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Behavioral health service request form. Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive. Only your provider can request a prior authorization to molina healthcare. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Prior authorization is not a.
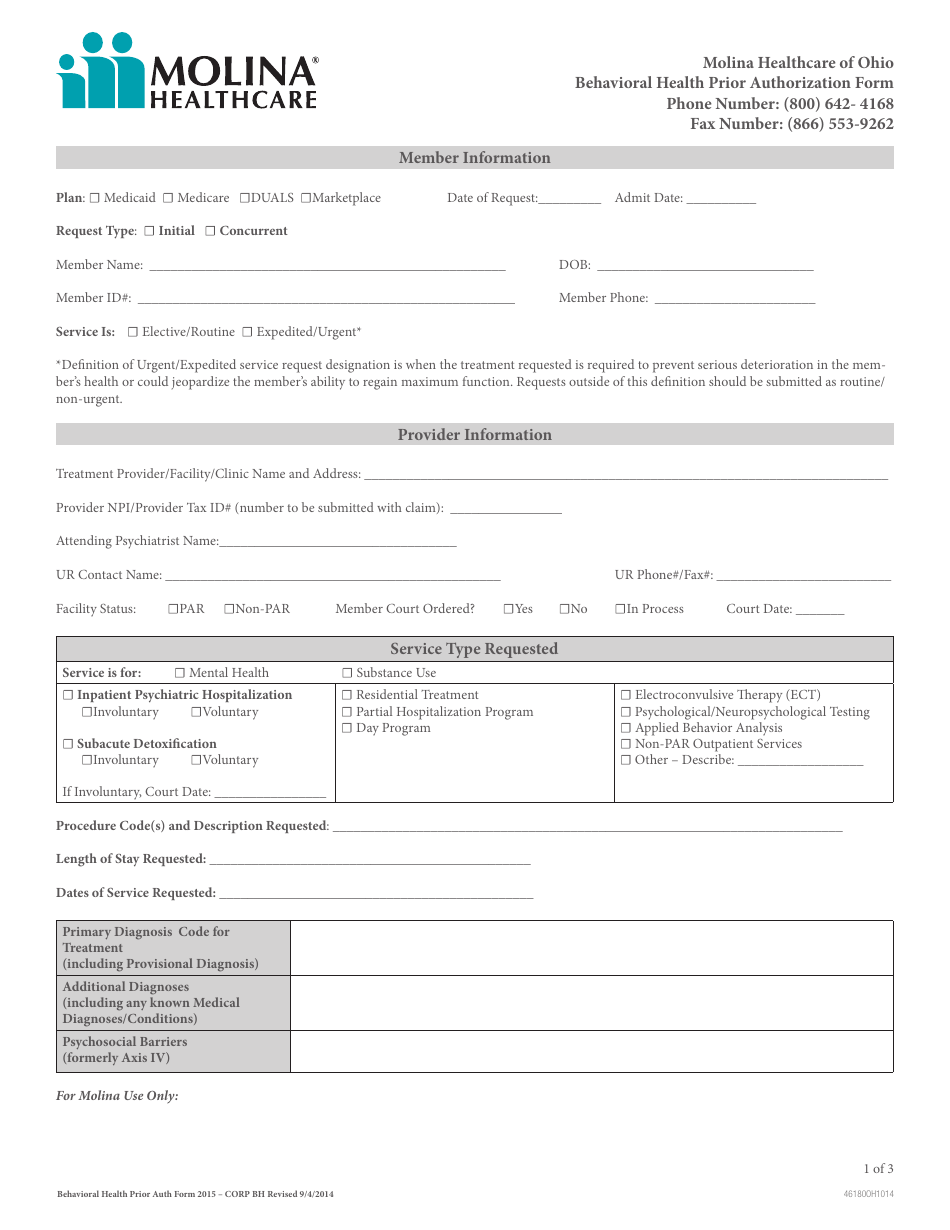
Ohio Behavioral Health Prior Authorization Molina Healthcare Download
Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. These tools provide a more efficient, clear process for the submission of. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone:.
Molina Prior Authorization Form Washington 2021 Fill Out and Sign
Prior authorization is not a. Molina healthcare will review the request and let the provider know if the service is approved. Web medicaid behavioral health and medical services prior authorization code matrix. Behavioral health service request form. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone:
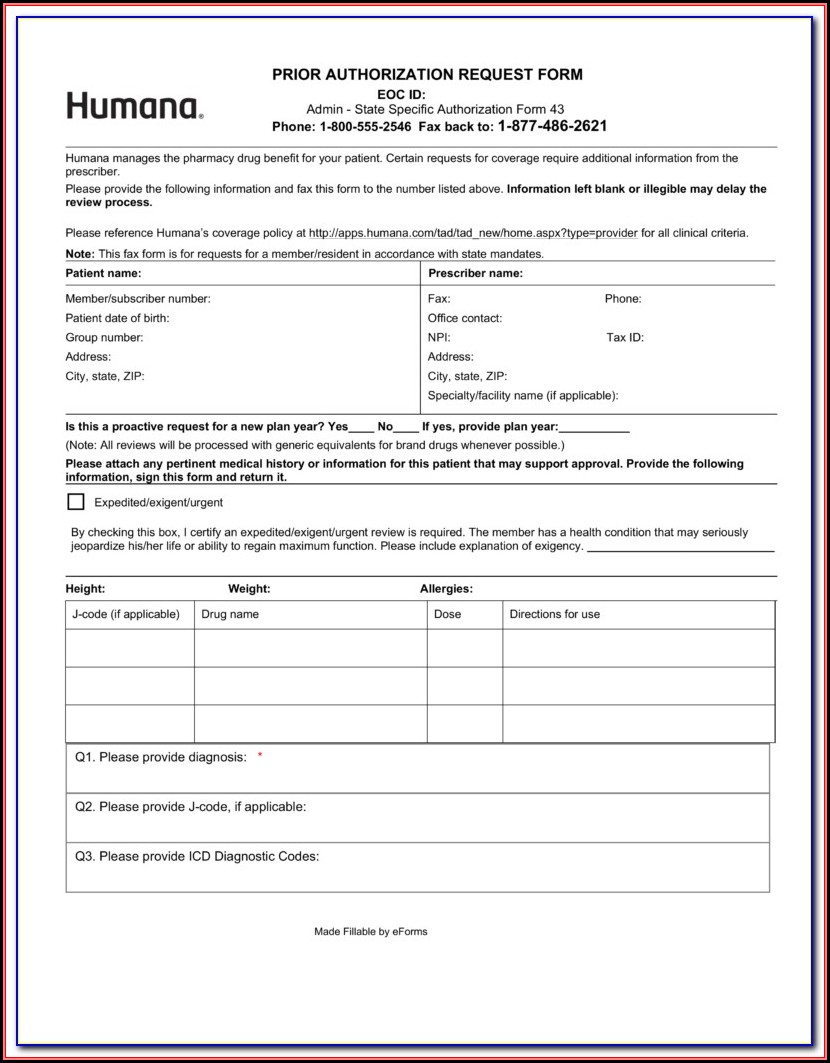
Web For Medicare Part B Drug Provider Administered Drug Therapies, Please Direct Prior Authorization Requests To Novologixvia The Molina Provider Portal.
Behavioral health service request form. Web o for medicare part b drug provider administered drug therapies, please direct prior authorization requests to novologix via the molina provider portal. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function.
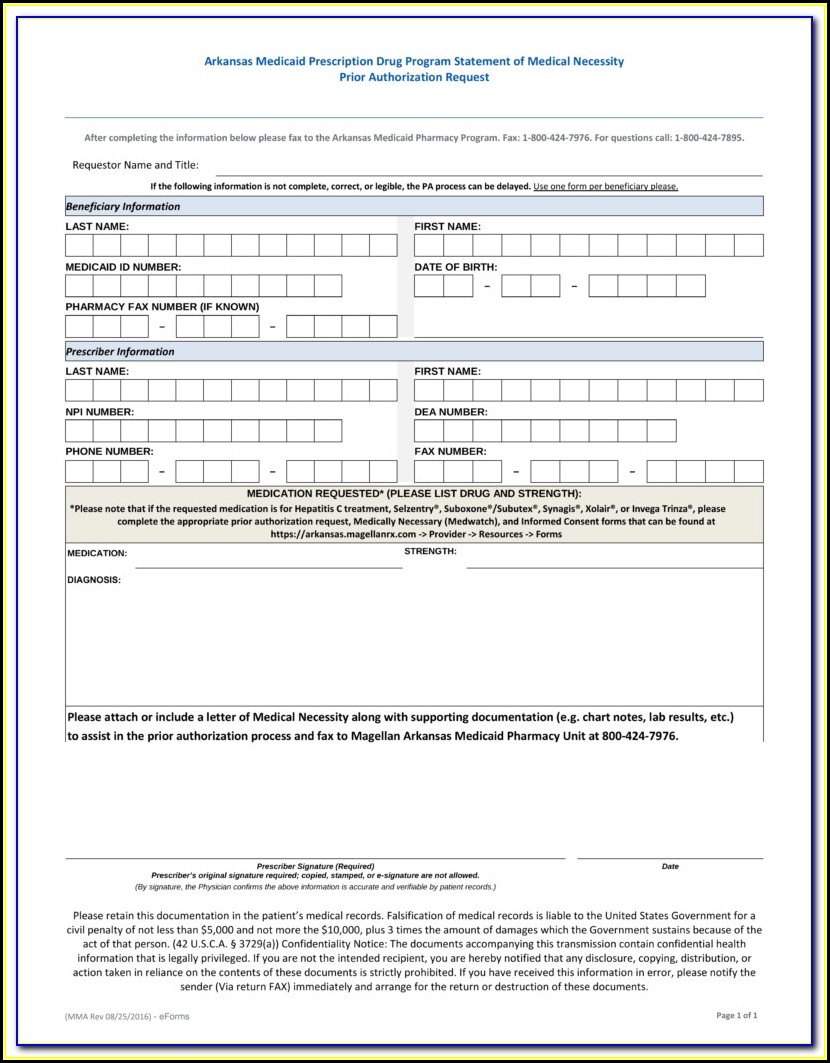
Web Medicaid Behavioral Health And Medical Services Prior Authorization Code Matrix.
Texas standardized prior authorization request form for healthcare services. Only your provider can request a prior authorization to molina healthcare. Prior authorization is not a. Molina healthcare will review the request and let the provider know if the service is approved.
Pharmacy And Outpatient Drug Services.
Web for a prior authorization, a provider must contact molina healthcare to request the services they would like you to receive. Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare prior authorization forms to the medicare provider page of. These tools provide a more efficient, clear process for the submission of.