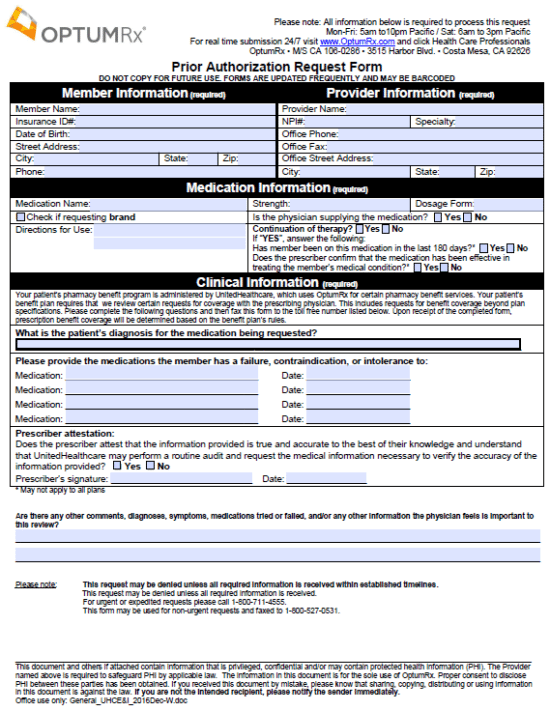
Prior Authorization Form For Optumrx
Prior Authorization Form For Optumrx - Web other ways to submit a prior authorization having difficulties with epa? Pt, saturday if you cannot submit requests to the optumrx® pa department through epa or telephone, click here. You can submit a verbal pa request. Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. All information below is required to process this request. Visit the portal to check prior auth information to determine if authorization is necessary for a particular service. Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. Web access the providers' prior authorization form to seek approval to prescribe medications for your patients in arizona, colorado, idaho, kansas city, nevada and utah. Web select the appropriate optumrx form to get started. •only be approved or effective for safely treating specific conditions
All information below is required to process this request. 5am to 10pm pacific / sat:. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web access the providers' prior authorization form to seek approval to prescribe medications for your patients in arizona, colorado, idaho, kansas city, nevada and utah. Web select the appropriate optumrx form to get started. Web prior authorization (pa), to ensure that they are medically necessary and appropriate for the reason prescribed before they can be covered. A list of tried and failed medication must be provided as a. Prior authorization (pa) requires your doctor to tell us why you are being prescribed a medication to determine if it will be covered under your pharmacy benefit. You can submit a verbal pa request. Web other ways to submit a prior authorization having difficulties with epa?
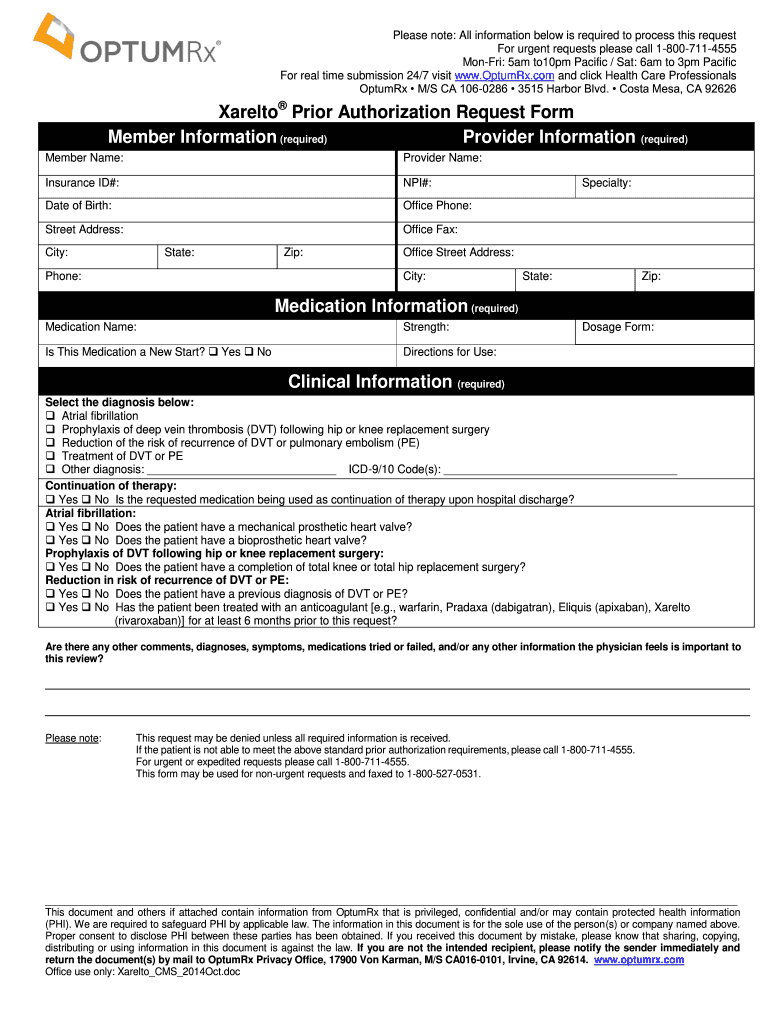
Web select the appropriate optumrx form to get started. Some medications must be reviewed because they may: Visit go.covermymeds.com/optumrx to begin using this free service. Web what is a prior authorization? Prior authorization (pa) requires your doctor to tell us why you are being prescribed a medication to determine if it will be covered under your pharmacy benefit. Web access the providers' prior authorization form to seek approval to prescribe medications for your patients in arizona, colorado, idaho, kansas city, nevada and utah. 5am to 10pm pacific / sat:. Web the optumrx prior authorization request form is a simple form to be filled out by the prescriber that requests that a certain treatment or medication be covered for a patient. Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. All information below is required to process this request.
Aarp Optumrx Prior Authorization Form Form Resume Examples EVKYM0oK06
Web what is a prior authorization? Web other ways to submit a prior authorization having difficulties with epa? Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. Visit go.covermymeds.com/optumrx to begin using this free service. All information below is required to process this request.
Aarp Optumrx Prior Authorization Form Form Resume Examples EVKYM0oK06
5am to 10pm pacific / sat:. Web what is a prior authorization? Web select the appropriate optumrx form to get started. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Visit go.covermymeds.com/optumrx to begin using this free service.
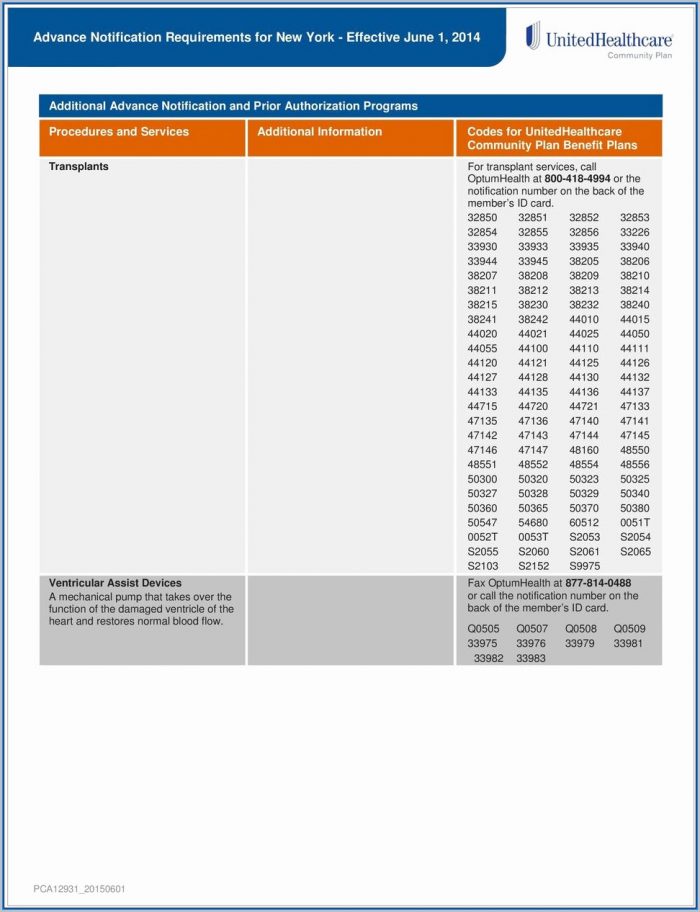
Prior Authorization Form For Medicare Advantage Universal Network
All information below is required to process this request. Visit go.covermymeds.com/optumrx to begin using this free service. Pt, saturday if you cannot submit requests to the optumrx® pa department through epa or telephone, click here. •only be approved or effective for safely treating specific conditions Visit go.covermymeds.com/optumrx to begin using this free service.
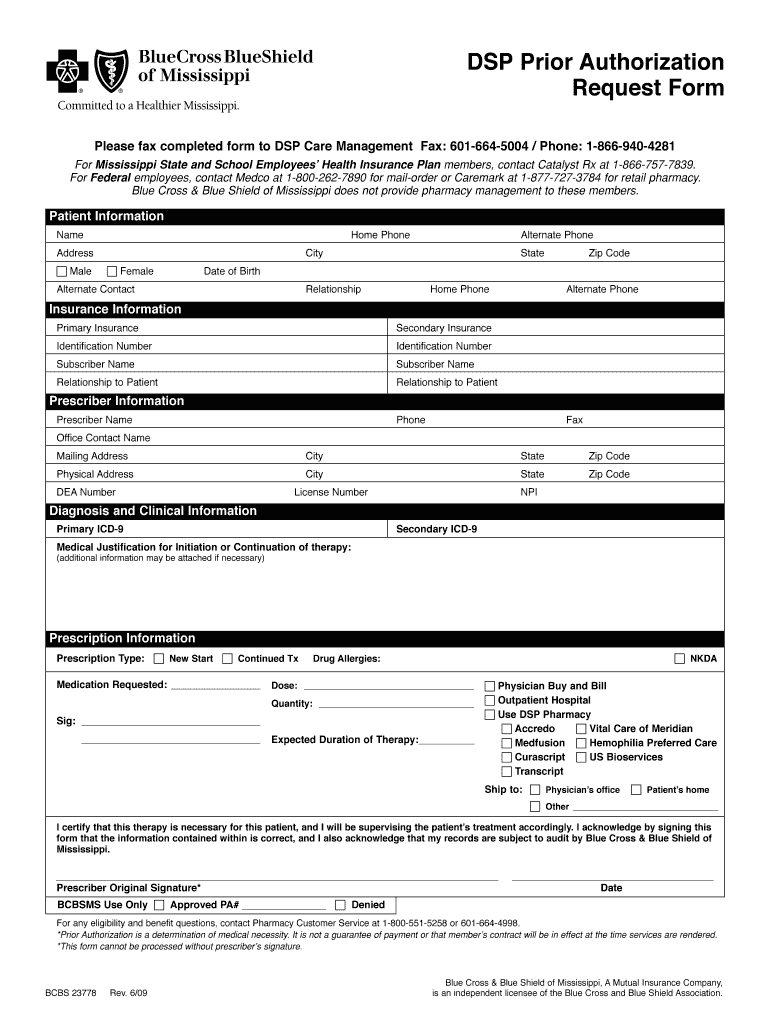
Wellpoint Pharmacy Prior Authorization Forms PharmacyWalls
Visit go.covermymeds.com/optumrx to begin using this free service. Some medications must be reviewed because they may: Web prior authorization (pa), to ensure that they are medically necessary and appropriate for the reason prescribed before they can be covered. Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. You can submit a verbal pa request.
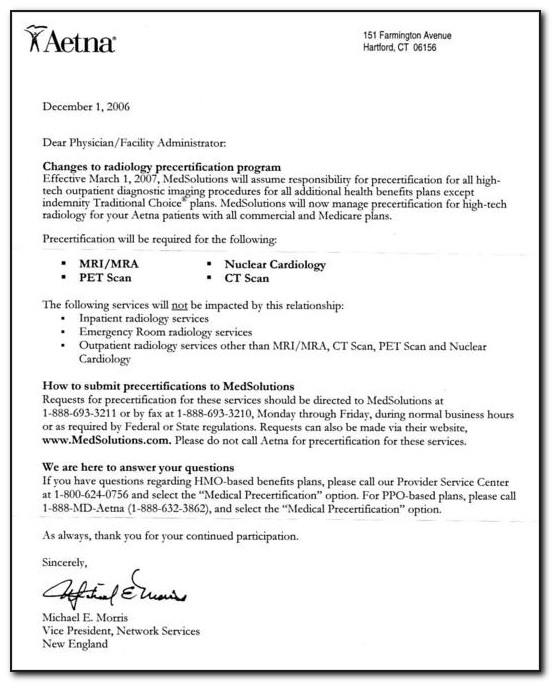
Aarp Medicarerx Plans United Healthcare Prior Authorization Form Form
Some medications must be reviewed because they may: Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Visit go.covermymeds.com/optumrx to begin using this free service. Visit go.covermymeds.com/optumrx to begin using this free service.
Medicare Part D Medco Prior Authorization Form Printable
Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. Prior authorization (pa) requires your doctor to tell us why you are being prescribed a medication to determine if it will be covered under your pharmacy benefit. •only be approved or effective for safely treating specific conditions You can submit a.
Optumrx Medicare Part D Electronic Prior Authorization form Fresh
5am to 10pm pacific / sat:. Pt, saturday if you cannot submit requests to the optumrx® pa department through epa or telephone, click here. Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. Web select the appropriate optumrx form to get started. Covermymeds is optumrx prior authorization forms’s preferred method.
Optumrx Medicare Part D Electronic Prior Authorization form Best Of
You can submit a verbal pa request. Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. A list of tried and failed medication must be provided as a. 5am to 10pm pacific / sat:. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review,.
Optumrx Prior Authorization Form Pdf 2021 Fill Online, Printable
Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. A list of tried and failed medication must be provided as a. Some medications must be reviewed because they may: 5am to 10pm pacific / sat:. Visit go.covermymeds.com/optumrx to begin using this free service.
Free OptumRX Prior Prescription (Rx) Authorization Form PDF
•only be approved or effective for safely treating specific conditions 5am to 10pm pacific / sat:. Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests. Visit the portal to check prior auth information to determine if authorization is.
Some Medications Must Be Reviewed Because They May:
Visit go.covermymeds.com/optumrx to begin using this free service. 5am to 10pm pacific / sat:. All information below is required to process this request. Web what is a prior authorization?
Web Other Ways To Submit A Prior Authorization Having Difficulties With Epa?
Visit go.covermymeds.com/optumrx to begin using this free service. Web access the providers' prior authorization form to seek approval to prescribe medications for your patients in arizona, colorado, idaho, kansas city, nevada and utah. You can submit a verbal pa request. Covermymeds is optumrx prior authorization forms’s preferred method for receiving epa requests.
A List Of Tried And Failed Medication Must Be Provided As A.
Pt, saturday if you cannot submit requests to the optumrx® pa department through epa or telephone, click here. Pas help manage costs, control misuse, and protect patient safety, as well as ensure the best possible therapeutic outcomes. Web select the appropriate optumrx form to get started. Prior authorization (pa) requires your doctor to tell us why you are being prescribed a medication to determine if it will be covered under your pharmacy benefit.
Web The Optumrx Prior Authorization Request Form Is A Simple Form To Be Filled Out By The Prescriber That Requests That A Certain Treatment Or Medication Be Covered For A Patient.
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. All information below is required to process this request. Web prior authorization (pa), to ensure that they are medically necessary and appropriate for the reason prescribed before they can be covered. Visit the portal to check prior auth information to determine if authorization is necessary for a particular service.