United Healthcare Bariatric Surgery Prior Authorization Form
United Healthcare Bariatric Surgery Prior Authorization Form - Refer to the back of the patient’s id card under the heading “prior authorization” for the appropriate contact information. Web in some cases, an approval is needed from your health plan before some health care services will be covered. Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the status of a. State policy/guideline indiana bariatric surgery (for. Web chpw’s bariatric surgery program. Chpw’s bariatric surgery program has three stages. Web after january 1, 2015, clients requesting the bariatric surgery program will need to request authorization for stages 2 and 3 from the client’s assigned managed care plan. Web sign in for a personalized view of your benefits. Your doctor is responsible for. This is called prior authorization.
Your doctor is responsible for. Web prior authorization and notification. Web in some cases, an approval is needed from your health plan before some health care services will be covered. Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the status of a. Web united healthcare bariatric surgery requirements. Web prior authorization requirements for louisiana medicaid effective general information. State policy/guideline indiana bariatric surgery (for. Web chpw’s bariatric surgery program. Web least six (6) consecutive months within the twelve months prior to authorization for surgery and at. Web here are some commonly used forms you can download to make it quicker to take action on claims, reimbursements and more.
Refer to the back of the patient’s id card under the heading “prior authorization” for the appropriate contact information. Web bariatric surgery (asmbs) textbook of bariatric surgery). Web least six (6) consecutive months within the twelve months prior to authorization for surgery and at. Web prior authorization and notification. Get the most out of your coverage. Unitedhealthcare community plan of washington process for skilled nursing facility;. Prior authorization for and successful completion of each stage is required. Web in some cases, an approval is needed from your health plan before some health care services will be covered. Chpw’s bariatric surgery program has three stages. Web united healthcare bariatric surgery requirements.
United Healthcare Primary Care Physician Referral Form Universal Network
Your doctor is responsible for. Web in some cases, an approval is needed from your health plan before some health care services will be covered. Get the most out of your coverage. Class iii obesity (body mass index greater than 40). State policy/guideline indiana bariatric surgery (for.
United Healthcare Dme Authorization form Elegant 10 Typical Reasons
This authorization may include your diet history and. Unitedhealthcare community plan of washington process for skilled nursing facility;. Web prior authorization requirements for louisiana medicaid effective general information. Chpw’s bariatric surgery program has three stages. Least three (3) office visits specifically relating to weight loss during the six (6).
Top 16 United Healthcare Prior Authorization Form Templates free to
Prior authorization for and successful completion of each stage is required. Web bariatric surgery (asmbs) textbook of bariatric surgery). Get the most out of your coverage. The american academy of sleep medicine (aasm) defines osa as a sleep related. This authorization may include your diet history and.
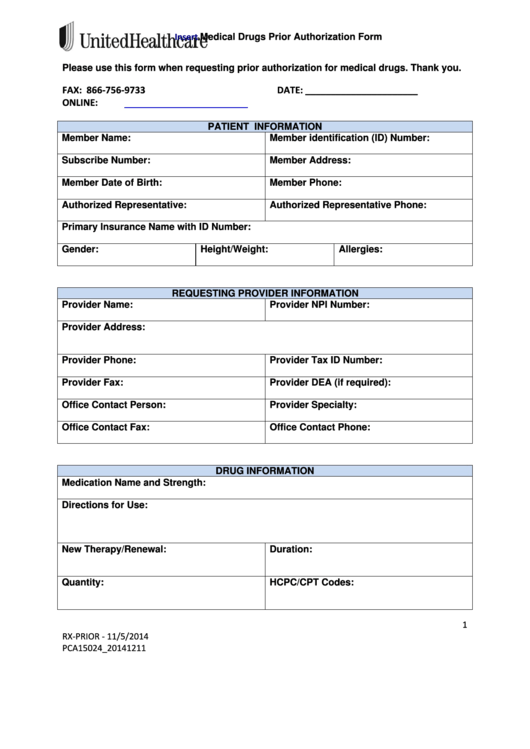
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
This list contains prior authorization requirements for unitedhealthcare. Get the most out of your coverage. Web prior authorization requirements for louisiana medicaid effective general information. Web disenrollment information declaration of disaster or emergency prescription drug formulary and other plan documents the plan documents search tool can help. Guide to united healthcare for.
Medicare Generation Rx Prior Authorization Form Form Resume
Chpw’s bariatric surgery program has three stages. Prior authorization for and successful completion of each stage is required. Web least six (6) consecutive months within the twelve months prior to authorization for surgery and at. Web after january 1, 2015, clients requesting the bariatric surgery program will need to request authorization for stages 2 and 3 from the client’s assigned.
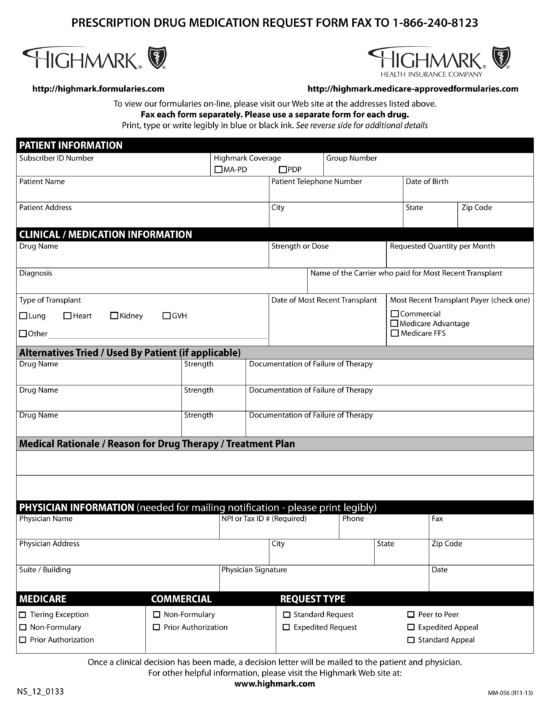
Free Highmark Prior (Rx) Authorization Form PDF eForms
This authorization may include your diet history and. Class iii obesity (body mass index greater than 40). Refer to the back of the patient’s id card under the heading “prior authorization” for the appropriate contact information. Least three (3) office visits specifically relating to weight loss during the six (6). State policy/guideline indiana bariatric surgery (for.
Pin on Bariatric Surgery Weight Loss Surgery
Prior authorization for and successful completion of each stage is required. Unitedhealthcare community plan of washington process for skilled nursing facility;. Least three (3) office visits specifically relating to weight loss during the six (6). Web view and download claim forms by following the link to the global resources portal opens in new window and clicking on my claims. Web.
(PDF) 2nd Registry Report of The United Kingdom National Bariatric
Unitedhealthcare community plan of washington process for skilled nursing facility;. Easy access to plan information anytime anywhere. Guide to united healthcare for. The american academy of sleep medicine (aasm) defines osa as a sleep related. Web after january 1, 2015, clients requesting the bariatric surgery program will need to request authorization for stages 2 and 3 from the client’s assigned.
WakeMed Bariatric Specialists of NC Referral Form Surgery NC
This is called prior authorization. Easy access to plan information anytime anywhere. All services are subject to member eligibility and benefit coverage. The american academy of sleep medicine (aasm) defines osa as a sleep related. Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the status of a.
United Healthcare Authorization Forms Fill Online, Printable
Web prior authorization and notification. Web view and download claim forms by following the link to the global resources portal opens in new window and clicking on my claims. Web in some cases, an approval is needed from your health plan before some health care services will be covered. Least three (3) office visits specifically relating to weight loss during.
Check Prior Authorization Requirements, Submit New Medical Prior Authorizations And Inpatient Admission Notifications, Check The Status Of A.
Unitedhealthcare community plan of washington process for skilled nursing facility;. Prior authorization for and successful completion of each stage is required. Web prior authorization requirements for louisiana medicaid effective general information. Class iii obesity (body mass index greater than 40).
This Authorization May Include Your Diet History And.
Web disenrollment information declaration of disaster or emergency prescription drug formulary and other plan documents the plan documents search tool can help. Web least six (6) consecutive months within the twelve months prior to authorization for surgery and at. Web after january 1, 2015, clients requesting the bariatric surgery program will need to request authorization for stages 2 and 3 from the client’s assigned managed care plan. Guide to united healthcare for.
This List Contains Prior Authorization Requirements For Unitedhealthcare.
This is called prior authorization. Web sign in for a personalized view of your benefits. Web bariatric surgery (asmbs) textbook of bariatric surgery). Chpw’s bariatric surgery program has three stages.
Easy Access To Plan Information Anytime Anywhere.
Least three (3) office visits specifically relating to weight loss during the six (6). Web chpw’s bariatric surgery program. All services are subject to member eligibility and benefit coverage. Refer to the back of the patient’s id card under the heading “prior authorization” for the appropriate contact information.