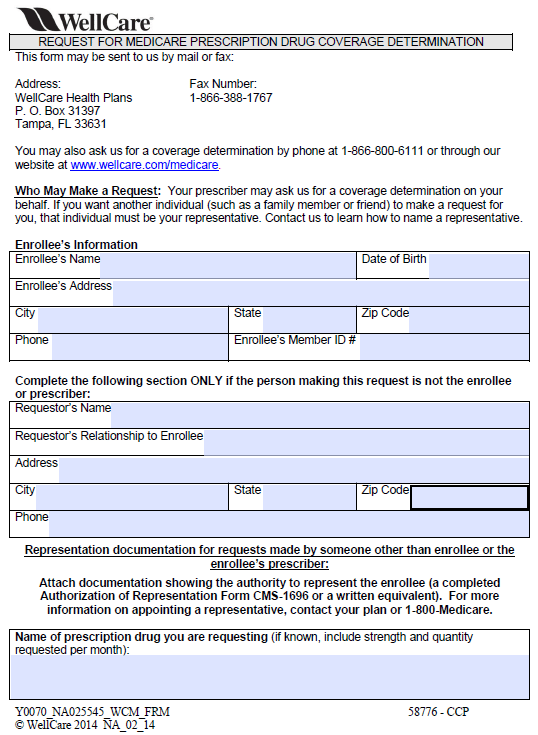
Wellcare Auth Form
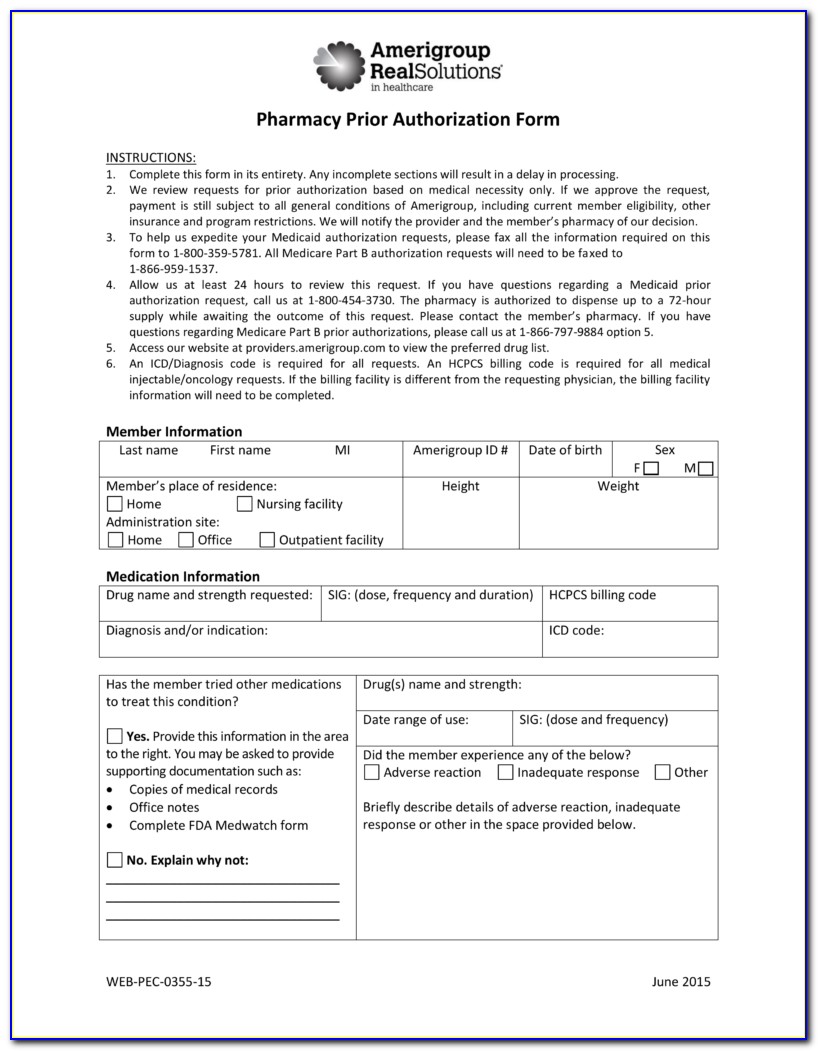
Wellcare Auth Form - The following information is generally required for all authorizations: An individual’s policy might not cover certain drugs, procedures, or treatments, and a wellcare prior authorization form allows them, or the. Web service authorization and referral requirements. If emergency services result in an inpatient hospital stay, hospitals must contact the member’s assigned ipa for authorization. Web submitting an authorization request. Web access key forms for authorizations, claims, pharmacy and more. The following information is generally required for all authorizations: You can even print your chat history to reference later! If you are having difficulties registering please click the “chat with an agent” button to receive assistance. Access key forms for authorizations, claims, pharmacy and more.
Disputes, reconsiderations and grievances ꮣꮢꮝꮤꮕꭹ ꭵꮏꭲ ꮧꭶꮃꮻꭹ ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ english provider payment dispute ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ. An individual’s policy might not cover certain drugs, procedures, or treatments, and a wellcare prior authorization form allows them, or the. Once you complete each authorization request, you can download or print a summary report for your records. Web you can submit two types of authorizations in the portal: If you are having difficulties registering please click the “chat with an agent” button to receive assistance. If you are referred to a specialist and he or she believes you need. A drug authorization is a request for prescription drug coverage. Drug authorizations are currently not available but will be at a later time. Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you. If emergency services result in an inpatient hospital stay, hospitals must contact the member’s assigned ipa for authorization.
Drug authorizations are currently not available but will be at a later time. You can even print your chat history to reference later! Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). Hospitals and ancillary providers must get prior authorization before providing any medical services to wellcare members, except for emergency services. Disputes, reconsiderations and grievances ꮣꮢꮝꮤꮕꭹ ꭵꮏꭲ ꮧꭶꮃꮻꭹ ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ english provider payment dispute ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). A drug authorization is a request for prescription drug coverage. >>complete your attestation today!<< access key forms for authorizations, claims, pharmacy and more. If emergency services result in an inpatient hospital stay, hospitals must contact the member’s assigned ipa for authorization.
46 Fresh Wellcare Prior Auth form Medication
>>complete your attestation today!<< access key forms for authorizations, claims, pharmacy and more. Once you complete each authorization request, you can download or print a summary report for your records. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent.
Wellcare Medicare Part D Coverage Determination Request Form Fill and
If you are referred to a specialist and he or she believes you need. Web access key forms for authorizations, claims, pharmacy and more. If emergency services result in an inpatient hospital stay, hospitals must contact the member’s assigned ipa for authorization. Hospitals and ancillary providers must get prior authorization before providing any medical services to wellcare members, except for.
Free Wellcare Prior Prescription (Rx) Authorization Form PDF
If you are referred to a specialist and he or she believes you need. Web submitting an authorization request. The following information is generally required for all authorizations: Access key forms for authorizations, claims, pharmacy and more. Drug authorizations are currently not available but will be at a later time.
Medicare Prior Auth Form For Medications Form Resume Examples
Web submitting an authorization request. Web access key forms for authorizations, claims, pharmacy and more. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). If you are having difficulties registering please click the “chat with an agent”.
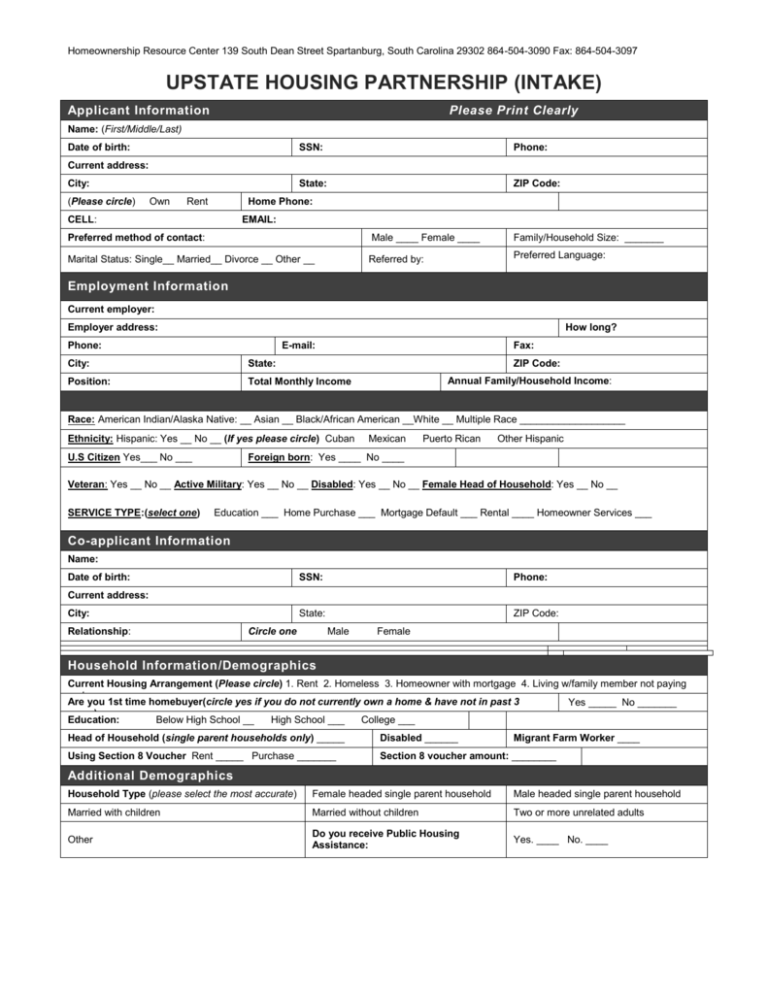
UHP Intake Form Upstate Housing Partnership
Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you. Access key forms for authorizations, claims, pharmacy and more. The following information is generally required for all authorizations: Once you complete each authorization request, you can.
PROGRAMA DE ACTIVIDADES DEL CENTRO PSICOPEDAGÓGICO ENEROJUNIO 2020
Web service authorization and referral requirements. If you are referred to a specialist and he or she believes you need. Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you. If you are having difficulties registering.
Wellcare Medicare Prior Authorization Forms
The following information is generally required for all authorizations: Once you complete each authorization request, you can download or print a summary report for your records. Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you..
Medicare Part D Prior Authorization form for Medication Lovely Wellcare
The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). You can even print your chat history to reference later! If you are referred to a specialist and he or she believes you need. The fastest and most.
Info Caremark Epa Form Fill Out and Sign Printable PDF Template signNow
A drug authorization is a request for prescription drug coverage. Web submitting an authorization request. Hospitals and ancillary providers must get prior authorization before providing any medical services to wellcare members, except for emergency services. An individual’s policy might not cover certain drugs, procedures, or treatments, and a wellcare prior authorization form allows them, or the. Drug authorizations are currently.
Wellcare Agent Resources Plans And Client Brochures
Web access key forms for authorizations, claims, pharmacy and more. You can even print your chat history to reference later! The following information is generally required for all authorizations: A drug authorization is a request for prescription drug coverage. Access key forms for authorizations, claims, pharmacy and more.
Hospitals And Ancillary Providers Must Get Prior Authorization Before Providing Any Medical Services To Wellcare Members, Except For Emergency Services.
The following information is generally required for all authorizations: If you are referred to a specialist and he or she believes you need. Disputes, reconsiderations and grievances ꮣꮢꮝꮤꮕꭹ ꭵꮏꭲ ꮧꭶꮃꮻꭹ ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ english provider payment dispute ꭱꮃꮧꮯ ꭶꮲꮝꭼꭲ. Web wellcare prior (rx) authorization form.
An Individual’s Policy Might Not Cover Certain Drugs, Procedures, Or Treatments, And A Wellcare Prior Authorization Form Allows Them, Or The.
Permission to see providers is called a referral and permission to receive services is called an authorization. if you need either type of permission, your primary care physician (pcp) will request it for you. Web service authorization and referral requirements. A drug authorization is a request for prescription drug coverage. Access key forms for authorizations, claims, pharmacy and more.
Drug Authorizations Are Currently Not Available But Will Be At A Later Time.
Web you can submit two types of authorizations in the portal: If you are having difficulties registering please click the “chat with an agent” button to receive assistance. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). If emergency services result in an inpatient hospital stay, hospitals must contact the member’s assigned ipa for authorization.
You Can Even Print Your Chat History To Reference Later!
The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). >>complete your attestation today!<< access key forms for authorizations, claims, pharmacy and more. Web submitting an authorization request. Once you complete each authorization request, you can download or print a summary report for your records.